The problem of organ deficiency for transplantation is urgent for all of humanity as a whole. About 18 people die every day due to the lack of organ and soft tissue donors, without waiting for their turn. Organ transplants in the modern world are for the most part carried out by deceased people who, during their lifetime, have signed the relevant documents confirming their consent to donation after death.
What is transplantation?

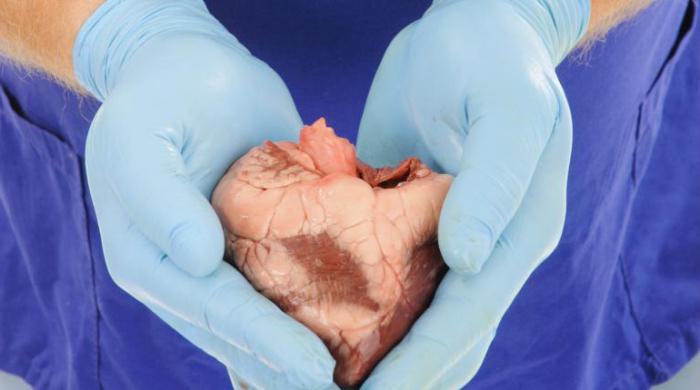
Organ transplantation is the removal of organs or soft tissues from a donor and transferring them to the recipient. The main direction of transplantology is the transplantation of vital organs - that is, those organs without which existence is impossible. These organs include the heart, kidneys, lungs. While other organs, such as the pancreas, can be replaced by replacement therapy. Today, great hopes for prolonging human life are given by organ transplantation. Transplantation is already successfully practiced. This is a transplant of a heart, kidney, liver, thyroid gland, cornea, spleen, lungs, blood vessels, skin integuments, cartilage and bones to create a skeleton with the aim that new tissues will form in the future. For the first time, a kidney transplant surgery to eliminate the patient’s acute renal failure was carried out in 1954, and the identical twin was the donor. Organ transplantation in Russia was first performed by academician B. Petrovsky in 1965.
What types of transplantation exist

All over the world there is a huge number of terminally ill people who need transplantation of internal organs and soft tissues, since traditional methods of treating the liver, kidneys, lungs, heart give only temporary relief, but do not fundamentally change the patient's condition. Organ transplantation is of four types. The first of them - allotransplantation - takes place when the donor and recipient belong to the same species, and xenotransplantation refers to the second type - both subjects belong to different species. In the case when a tissue or organ transplant is performed in identical twins or animals raised as a result of consanguineous crossing, the operation is called isotransplantation. In the first two cases, the recipient may encounter tissue rejection, which is due to the immune defense of the body to foreign cells. And in related individuals, the tissues usually take root better. The fourth type includes autotransplantation - a transplant of tissues and organs within the same organism.
Indications
As practice shows, the success of the operations is largely due to the timely diagnosis and accurate determination of the presence of contraindications, as well as how timely the organ transplant was performed. Transplantation should be predicted taking into account the patient's condition both before and after surgery. The main indication for the operation is the presence of incurable defects, diseases and pathologies that are not amenable to treatment by therapeutic and surgical methods, as well as life-threatening patients. When carrying out transplantation in children, the most important aspect is determining the optimal moment for the operation. According to experts of an institution such as the Institute of Transplantology, the postponement of the operation should not be carried out for an unreasonably long period, since the delay in the development of the young body can become irreversible. Transplantation is indicated in the case of a positive life prognosis after surgery, depending on the form of pathology.
Organ and tissue transplantation

In transplantology, autotransplantation is most common, as it eliminates tissue incompatibility and rejection. Most often, operations are performed on transplantation of skin, adipose and muscle tissues, cartilage, bone fragments, nerves, pericardium. Transplantation of veins and blood vessels is widespread. This was made possible thanks to the development of modern microsurgery and equipment for these purposes. A great achievement in transplantology is the transfer of fingers from the foot to the hand. Autotransplantation also includes transfusion of one’s own blood with large blood loss during surgical interventions. With allotransplantation, bone marrow, blood vessels, and bone tissue are most often transplanted . This group includes blood transfusion from relatives. Significantly rarely, brain transplant operations are performed, since so far this operation faces great difficulties, however, in animals, transplantation of individual segments is successfully practiced. Pancreas transplantation helps stop the development of such a serious disease as diabetes. In recent years, 7-8 of 10 operations performed have been successful. In this case, the entire organ is not completely transplanted, but only a part of it - islet cells that produce insulin.
Law on organ transplantation in the Russian Federation
On the territory of our country, the transplantology industry is regulated by the Law of the Russian Federation of 12.22.92 “On transplantation of organs and (or) human tissues”. In Russia, kidney transplantation, less often heart, liver transplantation is most often performed. Organ transplantation law considers this aspect as a way to preserve the life and health of a citizen. At the same time, legislation considers the preservation of the life of the donor in relation to the health of the recipient a priority. According to the Federal Law on Organ Transplantation, objects can be bone marrow, heart, lung, kidney, liver, and other internal organs and tissues. Organ harvesting can be carried out both in a living person and in a deceased person. Organ transplantation is carried out only with the written consent of the recipient. Only competent persons who have undergone a medical examination can be donors. Organ transplantation in Russia is free of charge, since the sale of organs is prohibited by law.
Transplant donors
According to the Institute of Transplantology, each person can become a donor for organ transplantation. For persons under the age of eighteen, parental consent for the operation is required. When signing a consent for organ donation after death, a diagnosis and medical examination are performed to determine which organs can be transplanted. Carriers of HIV, diabetes, cancer, kidney disease, heart disease and other serious pathologies are excluded from the list of donors for organ and tissue transplants. Related transplantation is carried out, as a rule, for paired organs - the kidneys, lungs, as well as unpaired organs - the liver, intestines, pancreas.
Contraindications to transplantation
Organ transplantation has a number of contraindications due to the presence of diseases that may worsen as a result of the operation and pose a threat to the patient’s life, including death. All contraindications are divided into two groups: absolute and relative. The absolute ones include:
- infectious diseases in other organs along with those that are planned to be replaced, including the presence of tuberculosis, AIDS;
- impaired functioning of vital organs, damage to the central nervous system;
- cancerous tumors;
- the presence of malformations and birth defects that are not compatible with life.
However, in the period of preparation for the operation due to treatment and elimination of symptoms, many absolute contraindications become relative.
Kidney transplant
Of particular importance in medicine is kidney transplantation. Since this is a paired organ, when it is removed from the donor, there are no disturbances in the functioning of the body that threaten his life. Due to the peculiarities of blood supply, the transplanted kidney survives well in the recipients. For the first time experiments on a kidney transplant were carried out in animals in 1902 by a scientist-researcher E. Ulman. During transplantation, the recipient, even in the absence of supporting procedures to prevent rejection of a foreign organ, lived a little more than six months. Initially, the kidney was transplanted onto the hip, but later, with the development of surgery, operations began to be performed to transplant it into the pelvic area, this technique is still practiced. The first kidney transplant was performed in 1954 between identical twins. Then, in 1959, an experiment was carried out on a kidney transplant with non-identical twins, while the technique to counter transplant rejection was used, and it proved its effectiveness in practice. New agents have been identified that can block the body’s natural mechanisms, including the discovery of azathioprine, which suppresses the body’s immune defenses. Since then, immunosuppressants have become widely used in transplantation.
Organ Preservation
Any vital organ that is intended for transplantation, without blood supply and oxygen, is subject to irreversible changes, after which it is considered unsuitable for transplantation. For all organs, this period is calculated in different ways - for the heart, time is measured in minutes, for the kidney - several hours. Therefore, the main task of transplantology is to preserve organs and maintain their performance right up to transplantation into another organism. To solve this problem, conservation is used, which consists in supplying the body with oxygen and cooling. In this way, you can save a kidney for several days. Preservation of the body allows you to increase the time for its study and the selection of recipients.
Each of the organs after its receipt must be subjected to conservation, for this it is placed in a container with sterile ice, after which they are preserved with a special solution at a temperature of plus 40 degrees Celsius. Most often, a solution called Custodiol is used for these purposes. Perfusion is considered to be carried out completely if a clean preservative solution without blood impurities emerges from the mouths of the graft veins. After that, the organ is placed in a preservative solution, where it is left until the operation.
Transplant rejection
When a transplant is transplanted into the recipient, it becomes the object of an immunological response of the body. As a result of the protective reaction of the recipient's immune system, a number of processes occur at the cellular level that lead to rejection of the transplanted organ. These processes are explained by the production of donor-specific antibodies, as well as antigens of the recipient's immune system. There are two types of rejection - humoral and super-sharp. In acute forms, both rejection mechanisms develop.
Rehabilitation and immunosuppressive treatment
To prevent this side effect, immunosuppressive treatment is prescribed depending on the type of operation performed, blood type, degree of compatibility of the donor and recipient, and the patient's condition. The least rejection is observed with a related transplantation of organs and tissues, since in this case, as a rule, 3-4 of 6 antigens coincide. Therefore, a lower dose of immunosuppressant drugs is required. The best survival is demonstrated by a liver transplant. Practice shows that the organ shows more than a decade of survival after surgery in 70% of patients. With prolonged interaction between the recipient and the transplant, microchemerization occurs, which allows over time to gradually reduce the dose of immunosuppressants until they are completely abandoned.