A positive analysis of feces for carbohydrates shows that not all carbohydrates are utilized in the digestive tract. This may be due to a lack of enzymes that break them down in the small intestine, or a violation of the composition of the microflora that metabolizes carbohydrates in the large intestine. Since milk is the only source of nutrients for infants, the state of lactose intolerance attracts the most attention in children under one year of age.
Carbohydrates, along with proteins and fats are the main components of food. They enter the digestive tract as part of products mainly of plant origin: fruits, vegetables, cereals, products containing flour, for example, bread, pastries, pasta. For breast-fed babies, the main carbohydrate is milk lactose. Artificial mixtures based on milk contain, in addition to lactose, sucrose as a sweetener.
Reducing sugars - lactose, maltose, glucose - are determined by chemical analysis for carbohydrates in feces.
In what cases is a study prescribed?
A routine study does not include stool analysis for carbohydrates. It is carried out only with the appearance of symptoms of intolerance to lactose, sucrose, glucose, galactose. Lactose intolerance is much more common than other types of intolerance.
Lactose intolerance
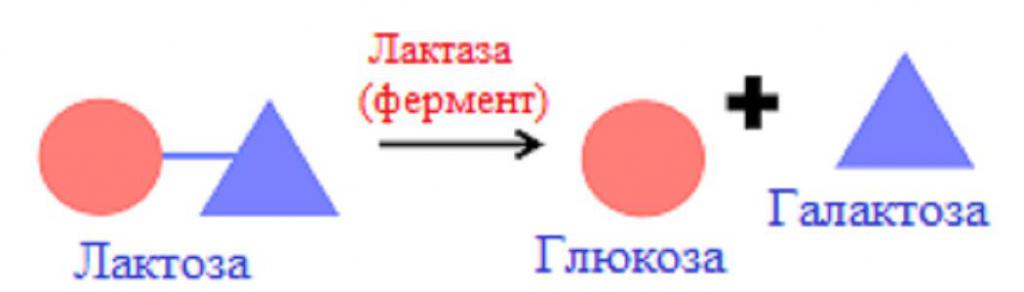
Lactose, or milk sugar, is the main carbohydrate in milk. It is a disaccharide formed by glucose and galactose residues. Lactose represents 90% of all milk carbohydrates.
Milk lactose, once in the small intestine, is broken down by the enzyme lactase to glucose and galactose. Lactase is the only enzyme in the body that acts on milk sugar. It is produced by the cells of the small intestine. Unsplit milk sugar moves further into the large intestine, where it is used by microflora, mainly lactobacilli. Thus, in the analysis of feces for carbohydrates in a child older than a year, lactose should not be detected.
In some cases, lactose does not break down in the small intestine. In the event that the lactase enzyme is not active enough or if its quantity is not enough to break down the incoming lactose, they speak of lactase deficiency. If the deficiency is minor, no symptoms occur. If lactase does not break down a lot of lactose, the disaccharide enters the large intestine in excess, it is detected during the analysis of feces for carbohydrates, and causes characteristic symptoms. This condition is called lactose intolerance. It can be caused by other reasons, for example, a decrease in the absorption of glucose and galactose in the intestine.
Causes of lactose intolerance in children
Reduced lactase activity is observed in 2/3 of children born. In most cases, this does not lead to the appearance of the disease. By 2-3 months of life, the enzyme begins to work in full force.
In full-term children up to a year in a predominant number of cases, lactose intolerance is caused by overfeeding, immaturity of the intestine and (or) its pathologies. In premature babies, low lactase activity is detected in almost everyone. Most often, it is in these cases that the doctor recommends taking an analysis of feces for carbohydrates.
Lactose intolerance during overfeeding is explained by an excess of milk sugar in the intestines of the child. Although the amount and activity of the enzyme is normal, they are not enough to break down the carbohydrate received with excess milk. Undigested lactose in large quantities is transported to the large intestine, which leads to the appearance of diarrhea and other characteristic signs. Most often, this condition is noted when feeding "on demand". Lactose overload is of particular importance in the development of symptoms in children born prematurely or undergoing hypoxia during childbirth. Dr. Komarovsky considers overfeeding to be the main reason for the diagnosis of lactose intolerance and the appointment of feces for carbohydrate content.
In children born at 28-30 weeks of gestation, the small intestine is not mature morphologically and functionally. Gradually, the gut matures and the enzyme activity normalizes.
Acquired (secondary) lactose intolerance is quite common. Its causes are most often acute intestinal infections: rotavirus, salmonellosis or the use of antibiotics and other drugs (anabolic steroids).
Signs of intolerance to lactose, sucrose and monosaccharides
Shortly after taking milk, there is discomfort, a feeling of bloating, rumbling in the abdomen, and stools sometimes liquefy. In infants, stools are usually watery, sour, yellow in color, foamy with a lot of gas. The main sign is diarrhea, although with minor hypolactasia, flatulence and intestinal colic may appear first. In infants, frequent regurgitation is observed due to an increase in intra-abdominal pressure. Appetite persists, weight is added slowly.
Advantages and disadvantages of the method
Analysis of feces for carbohydrates is widespread due to the low cost and ease of use. However, it has disadvantages:
- In infants, the microflora of the large intestine is only colonized, therefore, lactose is not utilized in the large intestine and it enters the feces more, sometimes the content exceeds 1%.
- The method does not allow to determine the content of individual carbohydrates: lactose, sucrose or glucose for the differential diagnosis of lactase, sucrose or other types of deficiency. It should be noted that lactase deficiency is much more common than other species.
Analysis
Determination of carbohydrates in feces is carried out by the Benedict reaction or using test strips. There are several reactions for the determination of reducing sugars, which include lactose: the Trommer, Felling and Benedict reaction and others. They are based on the ability of some sugars in an alkaline environment to reduce metals in the salt, which leads to a change in the color of the solution. The reaction with Benedict's reagent is the most sensitive, that is, it allows to detect a very low content of carbohydrates in the sample material.
An equal amount of Benedict's reagent is added to a few drops of stool centrifuge. The test tube is placed for several minutes in a water bath, after cooling, evaluate the result.
Analysis results
Benedict's reagent contains copper sulfate, the solution of which is blue. If there is no sugar in the feces, the reaction does not go, the mixture remains blue. If the stool contains lactose, it oxidizes the copper ion to red-brick copper oxide (I). A small amount of carbohydrates will lead to the formation of a small amount of reddish oxide, which is mixed with the blue color of the sulfate, resulting in a green color. A significant presence of carbohydrates gives a red color to the mixture. The laboratory assistant compares the resulting color with the colors of standard solutions. The table determines what carbohydrate content corresponds to this color. The result is given in% or g / l.
Interpretation of analysis results
Deciphering the analysis of feces for carbohydrates in infants :
- up to 2 weeks - no more than 1%,
- from 2 weeks to 6 months - 0.5-0.6%,
- from 6 months to a year - 0-0.25%,
- over a year - 0%.
For newborns up to 2 weeks of age, a result of 1% or lower is good, it indicates the formation of large intestinal microflora. A result greater than 1% is considered a deviation and requires a careful approach. Most likely, the analysis will need to be retaken.
For a child who is breastfeeding or artificial feeding from 2 weeks of age to 6 months, a good indicator is below 0.5-0.6%, indicating the absence of lactase deficiency. If the result is higher, lactase deficiency is possible. In children of this age, an increased content of carbohydrates in the feces is often noted, which often indicates the immaturity of the digestive tract. But even the identification of lactase deficiency should not become a reason for refusing breastfeeding. Since this condition is well treated while maintaining natural feeding with preparations containing enzymes.
In children older than one year, the result should be 0%. If it is higher, underutilization of lactose may be suspected. Most likely, the cause is a pathology of the intestinal tract or dysbiosis.
In children older than 3-5 years and adults, the result should be 0%. The increased result indicates, most often, intolerance to adult lactose, which occurs in 70% of the world's population.
Exceeding the norm is not a basis for making a diagnosis. Other studies are needed. Therefore, the decoding of the analysis of feces for carbohydrates should be done by the doctor.
Additional research
To make a diagnosis of lactase deficiency, the doctor first of all takes into account the clinical picture. Moreover, one or two manifestations of pathology are few. All clinical signs of failure should be present. Important information may be the presence of a similar pathology in the family, the disappearance of diarrhea when replacing milk with a dairy-free mixture.
The diagnosis is confirmed by additional laboratory tests:
- pH of feces less than 5.5;
- a positive analysis of the baby's feces for carbohydrates;
- the absence of an increase in the concentration of glucose in the blood after a lactose load.
The most informative test is the quantitative determination of lactase activity in the biopsy of the small intestine mucosa. But this is a painful, complex and expensive study, so it is usually not prescribed.