Bilirubin, or bile pigment, is a substance formed as a result of the breakdown of hemoglobin in liver cells. Normally, its concentration is in the range of 3.4–22.2 micromoles per liter. In this case, unconjugated bilirubin is 96, and direct - only 4 percent. An increase in its concentration occurs as a result of the destruction of hepatic cells, increased breakdown of hemoglobin, and failure of the outflow of bile from the liver. In some individuals, elevated bilirubin levels are caused by hereditary factors.
general information
In the cells of the liver and spleen during the splitting of red cells (red blood cells), one of the blood elements is released - hemoglobin, which then transforms into bilirubin. In an adult, about 250-350 mg is produced per day. Initially, plasma forms bilirubin in unconjugated form, bound to albumin (indirect, free bilirubin).
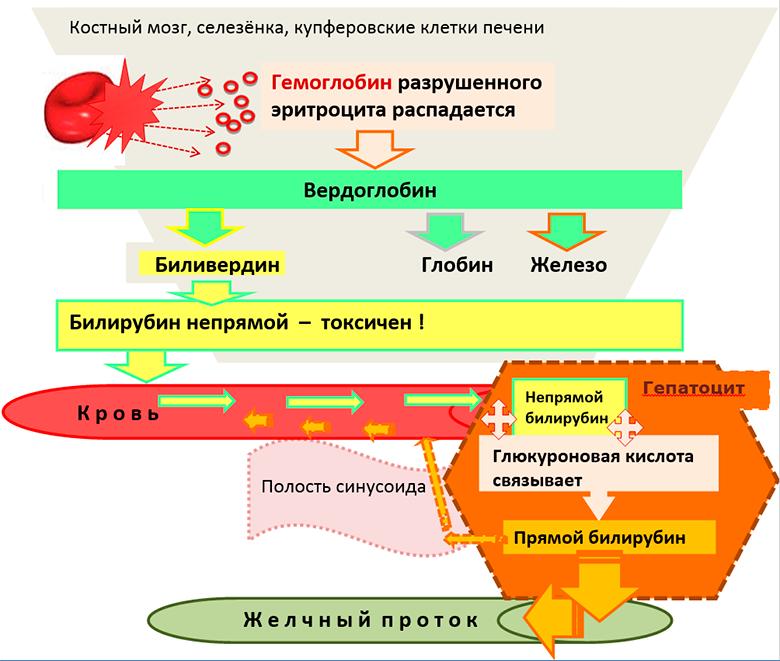
It is not able to leak through the kidney barrier. In the liver, bilirubin passes from albumin to the sinusoidal surface of the organ parenchyma cells, i.e., hepatocytes. In them, indirect bilirubin undergoes chemical reactions and is converted to conjugated, which penetrates the gallbladder or intestines, where it turns into urobilinogen. One part of this substance is absorbed in the small intestine and again enters the liver and is oxidized there. In the colon, bilirubin of bile turns into stercobilinogen. In the lower part of this gut, it oxidizes and acquires a brown tint and leaves with feces. A small part is absorbed into the bloodstream, then into the kidneys and excreted in urine. Free bilirubin enters the urine if its high serum content coincides with a violation of the permeability of the glomerular membrane.
Unconjugated bilirubin: structure, chemical properties
In its pure form, it is a crystalline substance having a red-brown or yellow-orange color, insoluble in water, the crystals of which are rhomboid-prismatic in shape. In another way, it is also called indirect or suprahepatic bilirubin, which is conjugated by liver enzymes before excretion. Before transportation, which is carried out by plasma, it binds most often with albumin.
In this form, it is transferred to other proteins. Under normal conditions, the connection between bilirubin and protein is very strong. However, fatty acids, hydrogen ions and some drugs can compete with bilirubin for binding to a protein. Due to its properties, suprahepatic bilirubin is not filtered in the glomeruli of the kidneys and is normally not found in urine. The structure of the trans form of unconjugated bilirubin is presented in the article.
Diagnostics
A blood test is performed to identify the negative effects of elevated bilirubin levels on the liver.
A blood test determines the amount of direct, indirect and total bilirubin. The terms “direct” and “indirect” came into use due to the reactions by which they are detected. To identify conjugated bilirubin, an Ehrlich reaction is performed. The pigment present in the blood reacts with the reagent, and to determine the free one, several operations are necessary, since it is insoluble in water.
The level of unconjugated bilirubin is the difference between total and associated pigment.
The determination of bilirubin in urine also has important diagnostic value and is one of the most sensitive and specific tests. In practical medicine, jaundice of a certain type in its pure form is quite rare, often it is a combination of different types. Therefore, in the diagnosis of hepatitis, this point should be taken into account. For example, with hemolytic jaundice, in which the level of indirect bilirubin rises, various organs are affected, including the liver. In this case, the patient shows signs of parenchymal hepatitis (direct bilirubin concentration increases in urine and blood).
Increased free bilirubin in newborns
This situation is observed in newborns in the first three days of life. In connection with the insufficient maturity of liver enzymes and increased decay of red blood cells with fetal hemoglobin, physiological jaundice occurs. If this condition is delayed in the baby, then the doctor is conducting studies to exclude the congenital pathology of the biliary tract and liver, hemolytic disease.

Rhesus conflict of mother and child provokes increased decay of red blood cells in the latter. As a result, unconjugated bilirubin rises. The negative consequences of this phenomenon is a toxic effect on the cellular tissue of the nervous system, which can lead to brain damage in the newborn (bilirubin encephalopathy). Hemolytic disease in newborns is subject to immediate treatment. In addition, hepatitis is detected in the crumbs with both an increased level of free and direct bilirubin. The causes of jaundice and the choice of treatment tactics are based on the clinical picture, as well as changes in the level of fractions of conjugated and unconjugated bilirubin. In INVITRO, whose laboratories are represented in many cities, at an affordable price you can take both a blood test and urine.
Factors Contributing to Hyperbilirubinemia
Often, an increase in bilirubin in the blood of an adult indicates health problems. However, among children, its increase is not always a pathology. For example, in newborns the reason for this phenomenon is physiological. Most diseases in which this indicator is above normal are acquired and respond to therapy. One of the main factors affecting the increase in unconjugated bilirubin is the low level of albumin proteins in the blood, as well as the inability of albumin to bind the bile pigment in full. Such medicines as cephalosporin antibiotics, penicillin series, as well as Furosemide, Diazepam, can provoke a rise in bilirubin in the blood. This phenomenon is due to the fact that the substances that make up the drug, competing with the pigment, bind to albumin.
The most common pathologies that occur against the background of an increase in the level of bile pigment in the blood are liver diseases, gall bladder, and other gastrointestinal organs.
As well as conditions in which there is an increased splitting of red blood cells.
Reasons for an increase in free bilirubin above the norm
An increase in unconjugated bilirubin is caused by some pathological processes in the body. A high release of free bilirubin occurs as a result of hemolysis, provoked by diseases such as:
- poisoning with toxins;
- malaria;
- genetic defects of red blood cells and hemoglobin;
- autoimmune processes in which red blood cells are involved;
- hemolytic anemia, both congenital and acquired.
In addition, liver tissue damage contributes to its increase in the following pathologies:
- all types of hepatitis;
- cirrhosis of the liver;
- leptospirosis;
- Infectious mononucleosis;
- liver damage as a result of prolonged use of certain medications;
- liver cancer;
- alcohol abuse.
Excessive bilirubin caused by hemolysis
If the cause of high bilirubin is associated with hemolysis, then the patient develops suprahepatic jaundice. The dermis acquires a light yellow hue. Against the background of an enlargement of the spleen, which is detected by ultrasound, the appearance of pain in the left side is possible. In the analyzes - a decrease in the number of red blood cells, a change in their shape and size.
Treatment is carried out both conservatively (enzyme and hormone therapy, immunosuppressants), and surgically. When there is a defect in red blood cells against the background of the disease, doctors recommend removing the spleen. The choice of medications directly depends on the cause of the pathology.
The increase in free bilirubin caused by damage to the liver tissue
Jaundice in this case is manifested by a yellow-saffron color of the mucous membranes and dermis. The palms acquire a red tint and the so-called spider veins appear on them. The liver is enlarged. Feces become colorless. With some long-term current diseases, varicose veins of the esophagus and stomach arise, and fluid accumulates in the abdominal cavity.
Indirect bilirubin
Unconjugated bilirubin dissolves well in fats, but it is not soluble in water. With urine, it is not excreted, since it is not able to pass through the renal filtration system. The rate of free bilirubin, which is measured in micromoles per liter, is in the range from 15.4 to 17.1. Its content in the body, of the total, is 96 percent.
Free bilirubin freely penetrates into cells, where it interacts with lipids of cell membranes, reaches mitochondria and causes a failure in them metabolic processes and cellular respiration, penetration of potassium ions through the cell membrane, and the creation of protein. Brain tissue is most susceptible to high levels of free bilirubin.
Conclusion
Unconjugated bilirubin, the formation of which occurs as a result of the breakdown of hemoglobin, is very toxic, readily soluble in cytolemma fats. Penetrating into it, he intervenes in the processes of cellular metabolism and disrupts them. It passes from the spleen to the liver together with albumin, where it interacts with glucuronic acid. As a result, a water-soluble, direct bilirubin appears, which has less toxicity.