Elimination of radicular lumbar and pain of other localization is considered today one of the most difficult, but at the same time, most important tasks. Observing the regression of pain, we can conclude that the correct therapy. In accordance with modern concepts of vertebrology, acute pain in the lower limbs or spine should be eliminated as soon as possible. With the transition of the condition to a chronic course, psychogenic disorders can occur. They, layering on general symptoms, complicate therapy and significantly worsen the prognosis. In this regard, specialists strive to use as short as possible and at the same time effective methods. One of these is paravertebral block. What it is, how it is carried out - more on this later in the article.
General information
Medical blockades are considered the most effective methods of eliminating pain and other manifestations of neurological pathologies. The procedures are based on the introduction of a drug into the outbreak. If compared with other methods of exposure (massage, physiotherapy, medication, acupuncture, manual therapy), then drug blockade has been used not so long ago - no more than a hundred years. However, during all this time, the procedures managed to establish themselves as a very effective way to eliminate pain. This is precisely the goal of the blockade. The pain must be eliminated quickly enough, with a minimum of side effects, time and material costs. It is precisely the method of therapeutic blockade that fully meets these conditions.
Description
The blockade is a temporary disconnection of one of the links from the arc of pain reaction. In addition to therapeutic, this procedure has diagnostic value. In some cases, the specialist finds it difficult to make an accurate diagnosis. This may be due to the fact that clinical manifestations are duplicated, or the relationship between symptoms and objective data is not clearly visible. It also happens that neurological signs are not confirmed by MRI. Or, conversely, CT scans or magnetic resonance imaging are not clinically justified. In such cases, selective blockade will be of great help in establishing an accurate diagnosis.
Features
If soreness is reduced by anesthesia of anatomical specific structures, this indicates that they are the source of pain. Separate selective injections are carried out at a particular site. This provides local anesthesia of the nerve, which supplies a certain area. An injection can also be made within the anatomical area, for example, an articular bag or joint. As a result, nocireceptors in this area are blocked. If corticosteroids are added to local anesthetics, selective injections in such cases can provide a longer therapeutic effect from anesthesia. Intra-articular administration of steroids helps to reduce inflammation and reduce the discomfort associated with it. Such injections are used in cases where the joints do not respond to the traditional effects - rest, drugs, physiotherapy. Blockade is used for myositis, radiculitis, neuralgia, sympathalgia. In addition to stopping pain, an improvement in neuro-trophic function is noted .
Benefits of the procedure
The rapid onset of relief is provided due to the direct penetration of the drug into the pathological focus and the effect of the drug on the endings and conductors that spread soreness. During the procedure, the likelihood of side effects is minimized. This is again due to the fact that the medication penetrates first into the focus of the pathology, and then only into the systemic circulation. With each new exacerbation of the syndrome, it is allowed to apply the blockade repeatedly. Practice has established a positive therapeutic effect of injections. Thanks to the use of blockade, muscle tension, vascular spasm are reduced, the inflammatory reaction and swelling in the pain focus are eliminated.
Paravertebral block
This concept should be considered collective. The term only indicates that the injection is carried out in the immediate vicinity of the spinal column. The injection can be intradermal, subcutaneous, perineural, intramuscular or radicular. In some cases, paravertebral blockade is used on the ganglia of the sympathetic borderline trunk. For example, a patient has a flattening disc. In this case, the approach of adjacent vertebrae and a decrease in the vertical diameter of the intervertebral foramen are noted . In the anterior sections, its size increases due to the development of osteophytes and other bone growths. A decrease in the diameter of the hole occurs with the development of spondylarthrosis, thickening of the yellow, interarticular ligament and other processes caused by osteochondrosis. Due to the fact that the leading nature of neurological disorders is compression and irritation of the cord, but not the infectious-inflammatory reactions of the membranes and roots, this variant of pathology is commonly called funicular. Based on this, the applied paravertebral block is funicular. Medicines are injected with a needle outward from the hole into the sagging cord, and not to the spinal root.
Classification
Therapeutic injections are divided into types according to the drug used and the area of influence. So, there are:
- Paravertebral blockade of the cervical spine.
- Injections for intercostal neuralgia.
- Thoracic paravertebral block.
- Piriformis muscle.
- At the lumbosacral level.
- The sciatic nerve and others.
The use of glucocorticoids
Paravertebral blockade with "Diprospan" is used for systemic collagenoses. A medication at the cellular level stops the development of inflammation. Before the introduction of the medicine, the area near the spinous process is chipped with anesthetics: the drug "Lidocaine" or "Novocaine". After that, the needle is replaced with a longer and thicker one and anesthesia is performed to the arch of the vertebra. After that, a mixture of anesthetic with the drug "Diprospan" is administered. Contraindications to the procedure include diabetes mellitus, thrombophlebitis, severe osteoporosis, psychosis, individual intolerance, infectious pathologies.
Use of anesthetic
Paravertebral novocaine blockade is a procedure, the essence of which is to introduce the drug into the zone of greatest pain. In particular, these areas include trigger points for overloaded joints and tense muscles, areas of passage of nerves and the location of their plexuses. Paravertebral blockade using an anesthetic can give a short effect (20-30 minutes). Nevertheless, even this time is quite enough to activate the normal tone of spasmodic muscles.
The effectiveness of the procedure and contraindications
The effectiveness is manifested by the removal of spasm throughout the muscle fiber, an increase in motor volume in the joint, a decrease in the intensity of pain sensitivity locally or in the area of innervation of the nerve root. Paravertebral blockade is not recommended, the technique of which will be described below, with severe bradycardia, weakness in the sinus node, atrioventricular blockade of the second / third degree (except cases when a probe is introduced to stimulate the ventricles), cardiogenic shock, arterial hypotension (severe), hypersensitivity . Contraindications include the presence of history of epileptiform seizures provoked by anesthetics, as well as impaired hepatic function.
Procedure
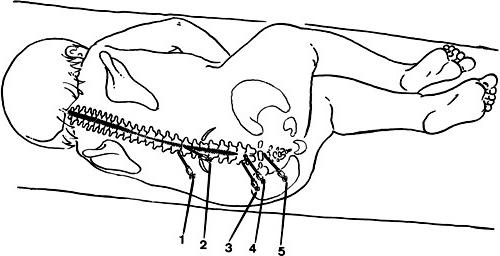
How are paravertebral blockades carried out? The technique of execution involves carrying out manipulations in a certain sequence. The patient is first laid on his stomach. By palpation, the site of maximum pain is determined. As a rule, this area corresponds to the projection of the cord that has suffered the most. Neurological tests are also used to help establish the place where the paravertebral block will be performed. The injection technique should be well established by a specialist.
The site is treated with alcohol or iodine. Using a thin needle, an anesthetic (Novocain) is injected into the area of the intended injection until a lemon peel forms. To get closer to the exit site of the cord, a second needle (longer) is inserted near the line of spinous processes (at a distance of 3-4 cm) in accordance with the desired interval. As it enters, 0.5% Novocaine solution is injected. The needle is inserted until it touches the transverse process. Further movement is bypassing it from below or above in the direction of the spine at an angle of 30 degrees. relative to the sagittal plane. The needle is inserted another 2 cm deep and 10-20 ml of anesthetic or hydrocortisone emulsion is injected. So, in general, paravertebral blockades are performed. The implementation technique involves the introduction of a needle in general 5-6 centimeters.
Acute cases
There are several methods by which paravertebral blockade is performed. The lumbosacral region is considered a rather problematic area, especially in acute pain and in the absence of a clear monoradicular syndrome. In this regard, injections from three points are effective. The introduction is between the vertebrae Liv and Lv, Lv and S1 and in the area of the first sacral opening. The injection of the drug "Hydrocortisone" in these zones is caused by the most frequent damage to the spinal cords. A patient may be given bilateral paravertebral block. The lumbosacral region in this case is cut off from six points. In accordance with the condition of the patient, the intensity and localization of pain, different dosages of the drug "Hydrocortisone" are used. When summing up to one cord (per 1 injection), 10-30 mg is used. With the proper implementation of the procedure, the pain is reduced or eliminated immediately after the administration of the medication. The blockade can be repeated if necessary. Repeated injection is allowed no earlier than after 2-3 days. After the procedure, the patient is recommended bed rest.
Other techniques
The patient takes a supine position. His head should be turned in the opposite direction from the area where the paravertebral block will be raised. The cervical region is considered the most mobile site. In this regard, this zone is injured more often than others. During the procedure, a 0.25% solution of anesthetic in a dose of 70-100 mg is used. An injection needle is inserted perpendicular to the skin surface closer to the outer border of the extensor extensor. Further, the movement is carried out until it comes into contact with a damaged vertebra or transverse process. After this, the needle moves 0.5-1 cm to the side. Subsequent injections are carried out at a distance of 1.5 cm from the previous ones. In some cases, a mixture of drugs "Novocaine" and "Hydrocortisone" is used. The last take 50-75 mg and bring the first to 100 ml.
Using Afonin Blend
This is another method of paravertebral lumbosacral blockade. 1.5-8 mg is injected to the site of exit of the cord from the opening (intervertebral). The total volume of the solution ranges from 30-80 ml. The dose depends on the number of points used in the blockade. The therapeutic course includes a single infiltration, if the result comes quickly enough. If the effect appears slowly, then apply 2-4 repeated blockades. Each subsequent injection is carried out 5-6 days after the last. Upon administration, the patient may experience various sensations in the area of innervation of the corresponding nerve fibers. For example, a patient may have a feeling of heaviness, paresthesia, pressure, aching pain.