The blood transfusion procedure (blood, plasma transfusion) cannot be taken carelessly. In order for the manipulation to bring the expected therapeutic benefit, it is important to choose the right donor material and prepare the recipient.
The success of this manipulation depends on a number of irreplaceable factors. A significant role is played by the thoroughness of the preliminary assessment of indications for blood transfusion, the correct phasing of the operation. Despite the development of modern transfusiology, it is impossible to exclude the risk of such a consequence of a blood transfusion as a fatal outcome with one hundred percent probability.
A brief history of manipulation
Since 1926, the Scientific and Research Center for Hematology, the leading scientific center of Russia, has been operating in Moscow. It turns out that the first attempts at blood transfusion were recorded in the Middle Ages. Most of them were unsuccessful. The reason for this can be called the almost complete lack of scientific knowledge in the field of transfusiology and the inability to establish group and Rhesus affiliation.
Transfusion of blood plasma with incompatibility of antigens is doomed to the death of the recipient, therefore, in our days, doctors have refused the practice of introducing whole blood in favor of implanting its individual components. This method is considered safer and more effective.
Risks to the recipient
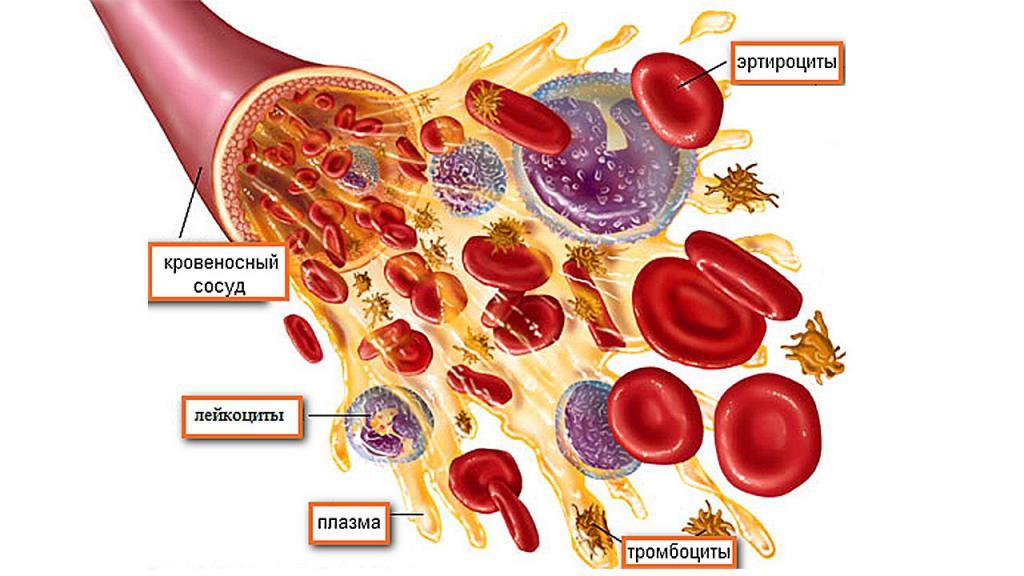
Even if the blood transfusion is somewhat reminiscent of the administration of saline or drugs by the drop, this procedure is more complicated. Blood transfusion is a manipulation equivalent to transplantation of biological living tissue. Implantable materials, including blood, contain many heterogeneous cellular components that carry foreign antigens, proteins, and molecules. Perfectly matched tissue will under no circumstances be identical with the patient’s tissue, so there is always a risk of rejection. And in this sense, the responsibility for the consequences of a blood transfusion lies solely with the specialist.
Any intervention carries risks that do not depend on the qualifications of a doctor or on preliminary preparation for the procedure. At the same time, at any stage of plasma transfusion (sample or direct infusion), the superficial attitude of the medical staff to work is unacceptable, the rush or lack of a sufficient level of qualification. First of all, the doctor must make sure that this manipulation is indispensable. If there are indications for a plasma transfusion, the doctor must be sure that all alternative methods of therapy are exhausted.
Who is indicated for blood transfusion
This manipulation has clear goals. In most cases, the infusion of donor material is due to the need to replenish the lost blood with extensive bleeding. Blood transfusion may also be the only way to increase platelet count to improve coagulation. Based on this, indications for blood transfusion are:
- deadly blood loss;
- shock state;
- severe anemia;
- preparation for planned surgical intervention, presumably accompanied by impressive blood loss and carried out using devices for cardiopulmonary bypass (heart surgery, blood vessels).
These readings are absolute. In addition to them, sepsis, blood diseases, chemical poisoning of the body can serve as a reason for carrying out blood transfusion.
Transfusion for children
There are no age restrictions for blood transfusion. With objective need, manipulation can be prescribed for a newborn. Blood transfusion at an early age has similar indications. In addition, when choosing a treatment method, a decision in favor of blood transfusion is made in case of rapid progression of the disease. In children of the first year of life, a blood transfusion can be caused by jaundice, an increase in the size of the liver or spleen, as well as an increase in the level of red blood cells.
The main arguments in favor of this manipulation are considered to be bilirubin. For example, if in a newborn it exceeds 50 μmol / l (material for research is taken from cord blood), the baby's condition is closely monitored, since this violation signals the need for the introduction of donor blood in the near future. Doctors monitor not only bilirubin levels, but also its accumulation rate. If it significantly exceeds the norm, the child is prescribed a blood transfusion.
Contraindications
Determination of contraindications is an equally important stage in the process of preparing for the procedure. According to the rules of blood transfusion, the main obstacles to this manipulation include:
- heart failure;
- recent myocardial infarction;
- coronary artery disease;
- congenital heart defects;
- bacterial endocarditis;
- hypertensive crisis;
- acute cerebrovascular accident;
- thromboembolic syndrome;
- pulmonary edema;
- glomerulonephritis at the acute stage;
- hepatic and renal failure;
- a tendency to allergies to many irritants;
- bronchial asthma.
In some cases, when transfusion is the only way to save a patient’s life, individual contraindications may be ignored. In this case, the tissues of the recipient and the donor must undergo many tests in order to confirm compatibility. Plasma transfusion should also be preceded by a comprehensive diagnosis.
Donated blood for allergy sufferers
For a person suffering from allergic reactions, different plasma transfusion rules apply. Immediately before manipulation, the patient must undergo a course of desensitizing therapy. For this, “Calcium Chloride” is administered intravenously, as well as the antihistamines “Suprastin”, “Pipolfen”, hormonal preparations. To reduce the risk of an allergic reaction to someone else’s biomaterial, the recipient is given the minimum amount of blood needed. Here the emphasis is not on quantitative, but on its qualitative indicators. In the plasma for transfusion, only those components that the patient lacks are left. In this case, the volume of fluid is replenished due to blood substitutes.
Transfusion biomaterial
The following can be used as transfusion fluid:
- whole donated blood, which is used extremely rarely;
- erythrocyte mass containing a scanty amount of leukocytes and platelets;
- platelet mass, which can be stored for no more than three days;
- freshly frozen plasma (they resort to transfusion in case of complicated staphylococcal, tetanus infection, burns);
- components to improve coagulation.
The introduction of whole blood is often impractical due to the high consumption of biomaterial and the highest risk of rejection. In addition, the patient, as a rule, needs specifically missing components, there is no sense in “loading” him with additional foreign cells. Whole blood is transfused mainly during open-heart surgery, as well as in emergency cases with life-threatening blood loss. The introduction of a transfusion medium can be carried out in several ways:
- Intravenous replacement of missing blood components.
- Exchange transfusion - part of the recipient’s blood is replaced with donor liquid tissue. This method is relevant for intoxications, diseases accompanied by hemolysis, acute renal failure. Most often, transfusion of freshly frozen plasma is carried out.
- Autohemotransfusion. Infusion of the patient’s own blood is implied. Such a liquid is collected during bleeding, after which the material is cleaned and preserved. This type of blood transfusion is relevant for patients with a rare group in which it is difficult to find a donor.
About compatibility
Transfusion of plasma or whole blood involves the use of materials of the same group, matching the Rhesus affiliation. But, as you know, any rule has an exception. If there is no suitable donor tissue, in an emergency, patients with group IV are allowed to inject blood (plasma) of any group. In this case, it is important to observe only the compatibility of Rh factors. Another interesting feature concerns the blood of group I: for patients who need to replenish the volume of red blood cells, 0.5 l of this liquid tissue can replace 1 liter of washed red blood cells.
Before the start of the procedure, personnel must verify the suitability of the transfusion medium, check the expiration date of the material, its storage conditions, and the tightness of the container. It is important to evaluate the appearance of blood (plasma). If the liquid contains flakes, strange impurities, convolutions, a film on the surface, it is impossible to introduce it to the recipient. Before the direct manipulation, the specialist must once again clarify the group and Rh factor of the blood of the donor and the patient.
Transfusion Preparation
The procedure begins with formalities. First of all, the patient should familiarize himself with the likely risks of this manipulation and sign all the necessary documents.
The next step is to conduct an initial study of the group affiliation and Rh factor of the blood according to the ABO system using tsiklon. The information received is recorded in a special register of the medical institution. Then, the seized tissue sample is sent to the laboratory to clarify blood phenotypes for antigens. The results of the study are indicated on the title page of the medical history. For patients with a history of complications of transfusion of plasma or other blood components, as well as pregnant and newborns, the transfusion medium is selected individually in the laboratory.
On the day of the manipulation, the recipient takes blood from a vein (10 ml). Half are placed in a tube with an anticoagulant, and the rest is sent to a container for a number of analyzes and biological samples. During transfusion of plasma or any other blood components, in addition to checking according to the ABO system, the material is tested for individual compatibility using one of the methods:
- conglutination with polyglucin;
- gelatin conglutations;
- indirect Coombs reaction;
- reactions on a plane at room temperature.
These are the main types of samples that are carried out during transfusion of plasma, whole blood or its individual components. Other tests are prescribed to the patient at the discretion of the doctor.
In the morning you can’t eat anything for both participants of the procedure. Blood transfusion, plasma is performed in the morning. The recipient is advised to empty the bladder and intestines.
How is the procedure
The operation itself is not a complex intervention that requires serious technical equipment. For exchange blood transfusion, punctured subcutaneous vessels on the hands. If there is a long transfusion, use large arteries - jugular or subclavian.
Before proceeding with a direct blood infusion, the doctor should not have the slightest doubt about the quality and suitability of the components being introduced. A detailed inspection of the container and its tightness, the correctness of the registration of accompanying documents, are mandatory.
The first step in blood transfusion is a single injection of 10 ml of transfusion medium. The liquid is introduced into the bloodstream to the recipient slowly, at an optimal speed of 40-60 drops per minute. After infusion of test 10 ml of donated blood, the patient's condition is monitored for 5-10 minutes. Biological test is repeated twice.
Dangerous signs that indicate the incompatibility of the biomaterials of the donor and the recipient are sudden shortness of breath, palpitations, severe redness of the skin of the face, decreased blood pressure, suffocation. If such symptoms appear, the manipulation is stopped and the patient is immediately given the necessary medical care.
If no negative changes have occurred, proceed to the main part of the blood transfusion. Simultaneously with the entry of blood components into the human body, it is necessary to monitor the temperature of his body, carry out dynamic cardiorespiratory monitoring, and control diuresis. The rate of administration of blood or its individual components depends on the indications. In principle, jet and drip introduction is allowed at a rate of about 60 drops every minute.
During a blood transfusion, a blood clot can stoke a needle. In this case, do not push the clot into a vein. The procedure is stopped, the thrombosed needle is removed from the blood vessel and replaced with a new one, which is already injected into another vein and the flow of liquid tissue is restored.
After transfusion
When all the necessary amount of donated blood enters the patient’s body, a little blood (plasma) is left in the container and it is stored in the refrigerator for two to three days. This is necessary in case the patient suddenly has post-transfusion complications. The drug will reveal their cause.
Basic information about the manipulation is recorded in the medical history. The documents indicate the volume of injected blood (its components), the composition, the result of preliminary tests, the exact time of the manipulation, a description of the patient's well-being.
After the procedure, the patient should not immediately get up. The next few hours will have to spend lying down. During this time, medical staff should carefully monitor the heartbeat, temperature readings. A day after the infusion, the recipient takes urine and blood tests.
The slightest deviation in well-being may indicate unforeseen negative reactions of the body, rejection of donor tissue. With increased heart rate, a sharp decrease in pressure and pain in the patient’s chest, they are transferred to the intensive care unit or intensive care unit. If during the next four hours after transfusion of plasma or other blood components the recipient does not increase body temperature, and the pressure and pulse readings are within the normal range, it can be said that the manipulation was successful.
What can be the complications
Subject to the correct algorithm and rules for blood transfusion, the procedure is absolutely safe for humans. The slightest error can cost a human life. So, for example, when air enters through the lumen of the vessels, embolism or thrombosis may develop, which are manifested by respiratory disorders, cyanosis of the skin, a sharp drop in blood pressure. Such conditions require emergency resuscitation, as they are deadly for the patient.
The post-transfusion complications mentioned above are extremely rare in life-threatening situations and often constitute an allergic reaction to the components of the donor tissue. Antihistamines help to cope with such.
A more dangerous complication with fatal consequences is the incompatibility of blood in the group and Rhesus, as a result of which the destruction of red blood cells occurs, multiple organ failure and death of the patient occurs.
Bacterial or viral infection during the procedure is a relatively rare complication, but its probability cannot be completely ruled out. If the transfusion medium was not stored in quarantine conditions, and when it was prepared, all the rules of sterility were not observed, the minimal risk of contracting hepatitis or HIV still occurs.