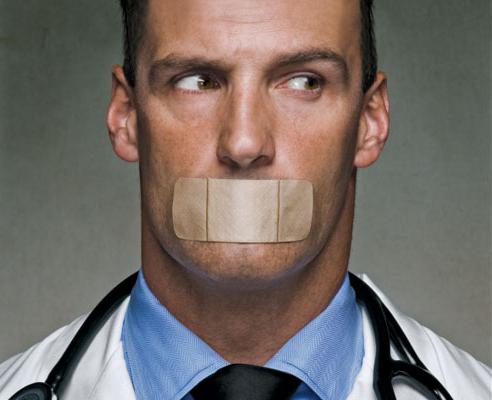
The development of the healthcare system in Russia is expected to significantly improve the quality of care. But not the least role is played by the regulation of the doctor-patient relationship, which so far, alas, remains in its infancy. And therefore, for many, medical secret is a mysterious and unclear concept.
Medical ethics
Doctors return their lost health to people, but at the same time they become carriers of various personal information that helps to treat the patient. A person will not openly talk about such matters with outsiders, and the doctor needs to be honest. The problem is that, as a rule, this is a stranger who does not want to trust such personal information without guarantees that it will not go further. How to be
Medical ethics, or deontology, comes to the rescue. It regulates the relationship between the doctor and the patient, and it is her staff who should be guided in various controversial issues. It is believed that the basic principles of medical deontology were formulated by Hippocrates in his famous oath.
Medical ethics includes questions of measures of responsibility for the health and life of patients, relationships with patients' relatives, as well as in the medical community as a whole, the admissibility of communicating with patients beyond the scope of business. But topics such as euthanasia and medical secrets have become more relevant in recent years. These are indeed very serious problems, but their solution should be regulated not only by morality. This is especially evident in the last question.
What is medical secret?
The definition of this concept is quite simple. A medical (medical) secret is all the information that a physician receives in the process of treating a patient and cannot transmit to third parties. It would seem that everything is unambiguous, but in reality everything is not so simple. Most patients have relatives, children, parents. After all, it is impossible for the mother of a one-year-old child to say that information about his health is not available to her? Or can the doctor keep silent about the fact that his patient, for example, has noticed signs of plague infection, because in this way he indirectly contributes to an epidemic? And what specific information is there no need to inform third parties? All these are complex ethical questions to which each person can offer his answers.
Fortunately, it has become clear quite a long time ago that it will not be possible to do without legal registration of these problems. Of course, this does not give a clear algorithm of actions in any situation, but it can set the framework on which to focus.
Legal regulation
The legislative basis of medical confidentiality comes from Art. 23, 24 of the Constitution of the Russian Federation, which protect the right to keep secret personal and family information. In addition, another legal act regulating the protection of information transmitted by a patient to a physician has entered into force relatively recently. This is federal law No. 323- dated 11/21/2011, which states what medical (medical) secrets are and what constitutes the information included in it. There is a judicial practice, although it is somewhat difficult to draw definite conclusions from its analysis - it is simply very small.

With regard to the state of affairs in this area in Europe and the USA, medical confidentiality and patient information are regulated somewhat differently. In America, there are no laws at the federal level; each state decides this issue in its own way. As for European states, the legal framework for protecting personal information, including medical confidentiality, is contained in the criminal codes, and their history goes back to the 17th century and earlier. Thus, to date, in some countries, for example, France and Germany, the regulation of the handling of information transmitted from the patient to the doctor is sufficiently detailed and specific.
What is included in confidential information?
A medical secret is, as it has already become clear, some personal information that the patient passes to his doctor. And the Russian legislation states what specifically compiles this information:
- the fact of contacting a medical organization;
- physical and mental health;
- diagnoses and forecasts;
- any other information reported by the patient or revealed during examination / treatment.
The main subjects, that is, persons accessing personal data, are employees of a medical institution, including trainees and pharmacists, as well as those who receive such information from doctors, for example, investigators and other law enforcement officials.
Nevertheless, under certain circumstances, the disclosure of medical information is completely legal. But they should be considered in more detail.
Access to personal data
Non-disclosure of medical secrets is generally the norm. However, there are circumstances in which information may be transferred to third parties. These include the following cases:
- Patient is less than 15 years old. In this case, information about his state of health is transmitted to his parents or legal representatives.
- Incapacity. The patient cannot express his will in connection with a physical or mental condition.
- There is a serious threat of the spread of an infectious disease.
- Investigation of accidents at work or in an educational institution.
- Transfer of information on bodily harm to law enforcement agencies.
- With written consent - for scientific research.
- Exchange of information between medical institutions.
- Quality control of the assistance provided.
- At the request of law enforcement.
In addition, in some cases, such information can also be accessed by relatives and relatives of the patient: with his written permission or without him, if he has not expressed a desire to the contrary, especially if the prognosis of his disease is extremely unfavorable. But medical ethics at the same time dictates the need to provide information in the most delicate form.
Disclosure Consequences
It seems, obviously, why medical secrecy is so important. The law protects the calm of citizens and punishes illegal access to information of a similar nature. It also provides for liability arising if confidentiality has not been respected:
- Disciplinary , that is, a remark or reprimand from the employer, in severe cases, dismissal with an entry in the workbook.
- Civil law - monetary compensation for the injured patient.
- Administrative (article 13.14 of the Administrative Code) - a fine of up to 5 thousand rubles.
- Criminal (part 2 of article 137 of the Criminal Code of the Russian Federation), the maximum sentence is imprisonment for up to 5 years.
About the timing
Current international and Russian legislation does not specify a specific period of time during which disclosure of medical secrets is impossible. Of course, this does not apply to the above exceptional cases. The only thing that legal acts define clearly is that the patient’s death is not a reason for disclosing information, so that medical confidentiality must be kept after its fact is established.
In Russia and abroad
In the post-Soviet space, unlike Europe and the USA, the legal regulation of access to medical information is still poorly developed. Despite the fact that the mentioned laws have already been introduced, their implementation is little controlled. At the same time, the introduction of an electronic card system and the complete rejection of paper records are both a field for abuse by medical personnel and the danger of breaking into databases and gaining access to personal data from outside. Probably, if the implementation matches the idea, the result will be excellent. But to talk about it is somewhat premature, especially when it comes to medical institutions included in the compulsory medical insurance system.