The children's organ that performs the immune function and the hematopoietic is the thymus. Why is it called children's? What happens to him in old age? And what is the clinical significance of this? You will find answers to these and many other questions in this article.
The role of the thymus in the human body
Thymus has a hematopoietic function. What does it mean? He is engaged in the differentiation and training (immunological) of T-lymphocytes. It is important that the "memory" of lymphocytes is very long, and therefore a child who has had the same chickenpox in 99% of cases will not get it again. This is called permanent immunity. In addition to the proliferation and differentiation of T-lymphocytes, the thymus is involved in the cloning of immune cells. By the way, I would like to note that a decrease in immunity to the thymus is directly related. A decrease in t-lymphocytes entails a cascade of reactions that lower immunity. And this explains a lot in pediatrics, when, for example, against the background of some commonplace disease, a secondary infection or a secondary disease occurs.
In addition, the thymus produces a number of hormones. These include: the thymic humoral factor, thymalin, thymosin, as well as thymopoietin. These hormones also perform an immune function.
Thymus: histology, structure, functions
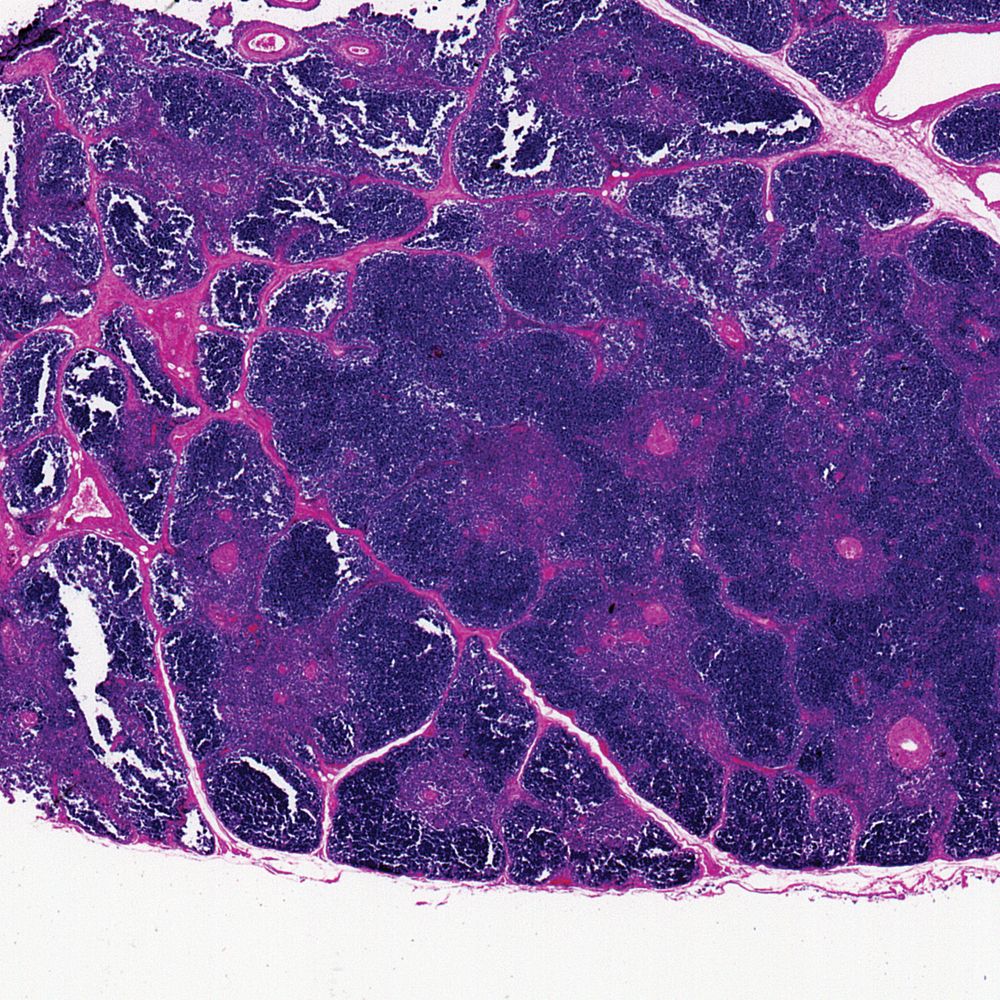
Thymus is a typical parenchymal organ (stroma and parenchyma are secreted in it). If you look at the appearance of the histological structure of the thymus, it can be noted that the organ is lobed.
In each lobule, a dark and bright zone is distinguished. Speaking in scientific language, it is a cortical and brain substance. As already mentioned, the thymus performs an immune function. Therefore, it can rightfully be called a bulwark of the children's immune system. So that this stronghold does not fall from the first foreign antigen protein that comes across, you need to create some kind of protective function for it. And nature created this protective function, calling it the hematotymic barrier.
Brief description of the histology of the thymic barrier
This barrier is represented by a network of sinusoidal capillaries and subcapsular epithelium. The composition of this barrier includes capillary epithelial cells. That is, antigens that are produced by pathogenic organisms immediately enter the bloodstream, and from there are spread throughout the human body. Thymus is no exception to where these antigens can get. How do they get there? They can get there through the microvasculature, that is, through the capillaries. The photo below shows the histology of the drug from the thymus, the vessels in the stroma are clearly visible.
Inside the capillary is lined with endothelial cells. They are covered with the basement membrane of the capillary. Between this basement membrane and the outer is the perivascular space. In this space there are macrophages, which are capable of phagocytizing (absorbing) pathogenic microorganisms, antigens, and so on. Behind the outer membrane are hundreds of lymphocytes and reticuloepithelial cells that protect the microcirculatory bed of the thymus from ingress of antigens and pathogenic microorganisms.
Thymic cortex
The cortical substance consists of a number of structures, for example, these are cells of the lymphoid series, macrophage, epithelial, supporting, "Nannies", stellate. Now let's look at these cells in more detail.
- Stellate cells - secrete thymic peptide hormones - thymosin or thymopoietin, regulate the growth, maturation and differentiation of T cells.
- Lymphoid cells - these include those T-lymphocytes that have not yet matured.
- Supporting cells - necessary to create some kind of framework. Most supporting cells are involved in maintaining the blood-thymus barrier.
- Cells "Nannies" - have in their structure recesses (invaginations) in which T-lymphocytes develop.
- Epithelial cells are the bulk of the cells of the cortical substance of the thymus.
- Macrophage cells are typical macrophages that have a phagocytosis function. They are also participants in the blood-thymus barrier.
The development of T-lymphocytes on a histological preparation
If you look at the drug from the periphery, then here you can find T-lymphoblasts that divide. They are located directly under the thymus capsule itself. If you go from the capsule in the direction of the brain substance, you can see already ripening, as well as fully matured T-lymphocytes. The entire development cycle of T-lymphocytes takes approximately 20 days. In the process of development, they have a T-cell receptor.
Once the lymphocytes have matured, they interact with epithelial cells. Here selection is made according to the principle: suitable or unsuitable. Next, the differentiation of lymphocytes occurs. Some will become T-helpers, while others will become T-killers.
What is it for? Each T-lymphocyte interacts with different antigens.
Approaching the medulla, already matured T-lymphocytes that have passed differentiation are tested according to the danger principle. What does it mean? Can this lymphocyte harm the human body? If this lymphocyte is dangerous, then apoptosis occurs with it. That is, the destruction of the lymphocyte. In the brain substance are already matured, or ripening T-lymphocytes. These T cells subsequently enter the bloodstream, where they disperse throughout the body.
The thymus medulla is represented by protective cells, macrophage structures and epithelial. In addition, there are lymphatic vessels, blood vessels and Gassal's bodies.
Development
The histology of the development of the thymus is very interesting. Both diverticulum starts from 3 branchial arches. And both of these strands grow into the mediastinum, most often the anterior. Very rarely, the stroma of the thymus gland is formed by additional cords of 4 pairs of gill arches. Lymphocytes are formed from blood stem cells, which will then migrate from the liver to the bloodstream, and then to the thymus of the fetus. This process occurs in the early stages of fetal development.
Analysis of the histological preparation
A brief histology of the thymus is as follows: since it is a classic parenchymal organ, it examines the laboratory assistant first stroma (organ frame), and then the parenchyma. Inspection of the drug is first done at a large increase in order to view and navigate the organ. Then they switch to a large increase for examination of tissues. The stain of the drug is most often hematoxylin-eosin.
Thromb stroma
Outside the organ is a connective tissue capsule. It covers the organ from all sides, giving shape. Connective tissue septa pass inside the organ from the connective tissue capsule; they are also called septa, which divide the organ into lobules. It is worth noting that the connective tissue capsule and connective tissue septa consist of a dense, formed connective tissue.
The influx or outflow of blood to the organ is carried out through blood vessels. These vessels also pass in the elements of the stroma. Distinguishing an artery from a vein is very simple. First, the easiest way to do this is by the thickness of the muscle layer. The artery layer of muscle tissue is much thicker than the vein. Secondly, the choroid of the vein is much thinner than that of the artery. Below in the photo, the histology of the thymus can be seen on the drug.
To consider the elements of the stroma inside the lobule, you need to go to a large increase. So the laboratory assistant can see reticular epithelial cells. By their nature, these cells are epithelial, have processes that bind to each other. Thus, the cells retain the thymus framework from the inside, as they are tightly connected with the elements of the parenchyma.
The lab technician most often will not see the cells of the reticuloepithelial tissue themselves, since they are hidden by numerous layers of the parenchyma. Thymocytes are so tightly adjacent to each other that they overlap stromal cells. But in a single order, you can still see between the thymocytes in the bright lumens of the oxyphilic-stained cells. These cells have large nuclei that are arranged in a chaotic manner.
Thymus parenchyma
Thymus parenchyma should be considered in a single lobule. Therefore, the laboratory assistant after examining the stroma returns to a small increase. When the laboratory assistant returned to the starting position, he sees a sharp contrast. This contrast indicates that each lobule consists of cortical and medulla.
Cortical substance
It is worth noting that the thymus parenchyma is represented by lymphocytes. In the cortical substance, which is colored violet on the preparation (basophilic color), the lymphocytes are closely located relative to each other. In addition to the elements of the stroma and lymphocytes, the laboratory assistant will not see anything else in the cortical substance.
Brain substance
In the medulla, oxyphilic coloration predominates, rather than basophilic, as in cortical. This is because the number of lymphocytes decreases sharply, and they are less often located relative to each other. Among the lymphocytes in the brain, thymic bodies can be seen. These structures in textbooks are often called the bodies of Gassalle.
Gassal bodies on the preparation are formed by twisted structures. In fact, these are ordinary dead, keratinizing fragments of the stroma - those same epithelial reticulocytes. Gassal's bodies are oxyphilically painted elements of the brain part of the thymus.
Very often, students differentiate the thymus preparation in histology according to Gassal's bodies. They are a characteristic feature of the drug, always located exclusively in the medulla. Below on a photo these thymic little bodies are presented.
If the bodies do not have swirling red structures, then Gassal's bodies look like just white spots. Sometimes they are compared with the voids (artifacts) of the drug, which often form during its preparation. In addition to resembling artifacts, thymic bodies are similar to vessels. In this case, the laboratory assistant looks at the presence of the muscle layer and the presence of red blood cells (if the latter are absent, then this is the thymus body).
Thymus involution
As stated at the beginning of the article, the thymus is a child’s gland. Of course, this is not entirely true, but the presence of an organ does not always mean that it functions.
When the child reaches one year of age, then at this moment there comes a peak in the production of lymphocytes, respectively, and the work of the gland. After gradually, the thymus is replaced by adipose tissue. By the age of twenty, half of the thymus consists of adipose and lymphoid tissue. And by the age of fifty, almost the entire organ is represented by adipose tissue. This involution is associated with the fact that T-lymphocytes have a lifelong memory that accompanies the human body throughout his life. As the number of T lymphocytes in the blood becomes sufficient, the thymus simply remains the organ that "maintains" the constancy of T lymphocytes in the blood.

The involution of the histology of the thymus can occur much faster due to provoking factors. These factors can be acute infectious diseases, chronic diseases, radiation, etc. Due to these factors, the level of cortisone and hormones of a steroid nature significantly increases in the blood, they destroy the immature T-lymphocytes, thereby destroying the thymocytes themselves, replacing them with adipose tissue.