There is nothing superfluous in our body - Mother Nature took good care of this. Although, as some have noted, such an organ as the appendix is not of particular value, and it is quite possible to fully live without it. But this is not about this, but about the important role the lumbar plexus plays, or plexus lumbalis. The concentration of nerve endings of the pelvic region and lower extremities is concentrated here.
The inflammatory processes occurring in this area are accompanied by neuralgia, which covers the lower half of the body. Often, pain appears. To clearly understand how pathological processes occur, you need to know the anatomy of this department well.
Definition
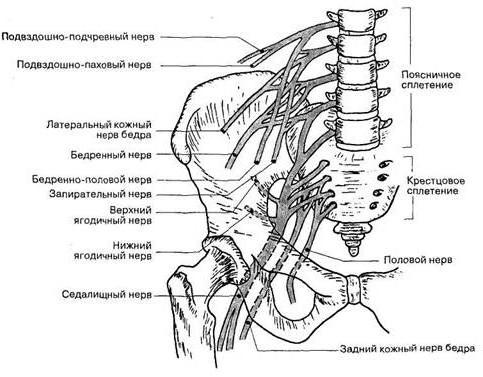
The lumbar plexus is the combination of several types of nerves. The first three of the spinal nerves take part in its formation. In part, this may also include 12 branches of the thoracic and 4 branches of the spinal nerve endings. Large muscle fibers are where the lumbar plexus is located. Anatomy involves finding the nerve branches in front of the transverse processes of the lumbar vertebrae.
These nerve endings are responsible for the innervation of certain parts of the muscle fibers, including the skin of the peritoneum. In addition, they are associated with the skin surface of the external genitalia, the medial surface of the lower leg, and the anteromedial side of the thigh. In total, in this section, several types of nerve endings can be distinguished:
- iliac-hypogastric;
- ileo-inguinal;
- femoral genital;
- lateral;
- obturator;
- femoral.
Let's consider in more detail what they are and where they lie. Conventionally, all nerves can be divided into two triples.
The first three nerves
The iliac-hypogastric nerves of the lumbar plexus are formed from the anterior 12 thoracic and 1 lumbar branches of nerve endings. From them, they pass through the large lumbar muscle and then come in contact with the front surface of the square muscle of the lower back, thus being near the kidney. Further, the nerve runs from top to bottom, keeping its direction from back to front. On the way to the iliac crest, it penetrates the transverse abdominal muscle and then lies between it and the internal oblique muscle fibers of the abdomen. The further path lies already between both oblique muscles.
In the deep inguinal ring, the iliac-hypogastric nerve also permeates the internal oblique muscle and the wide tendon plate of the external oblique muscle. After that, it branches into skin processes of the abdominal wall above the pubic joint. Its function includes the innervation of most of the abdominal muscles. Also, nerves pass through the skin in the thigh, buttocks, anterior abdominal wall above the pubis.
Another branch, which originates from the anterior nerve root, but is located slightly lower than the previous one, is called the ileo-inguinal nerve, which also enters the lumbar plexus. Its anatomy is different for men and women. In the stronger sex, the nerve passes through the inguinal canal and breaks up into small skin branches on both surfaces of the thigh near the scrotal nerve cells. The latter are responsible for the innervation of the skin of the genital organ and partially the scrotum. In women, these same endings connect the central nervous system with the skin on the pubis and large labia.
The femoral-genital pierces the large lumbar muscle and is even divided into two branches - the genital and femoral. The genital, otherwise called the seminal nerve, is directed downward and, like the spermatic cord, passes through the inguinal canal. In the male body, it is associated with the muscle that is responsible for raising the testicle, the skin of the scrotum, as well as the fleshy membrane and the surface of the skin of the superior medial thigh. The female lumbar nerve plexus is arranged differently - the nerve paired with the round ligament of the uterus of the inguinal canal and then goes to the skin of the labia majora.
The second femoral branch from this common ending is directed downward and runs laterally from the external iliac artery directly beneath the inguinal ligament. Below her nerve is divided into branches of the skin surface of the thigh.
The second three nerves
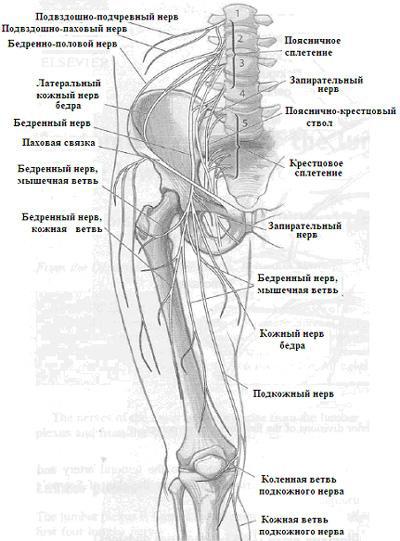
Below all three of these nerves are three larger branches. These are lateral, femoral and obstructive nerve endings. The first of the list is located on the side of the inguinal ligament. It can be on the surface or inside the tailor muscle, being under the connective tissue membrane. The nerve is responsible for the sensitivity of the lateral surfaces of the buttocks just further than the greater trochanter of the femur and closer to the lateral surface of the thigh.
Continuing to analyze how exactly the lumbar plexus is formed, it is worth moving to the obturator nerve. It goes down along the large lumbar muscle, more precisely, along its edge and enters the pelvic area. Joining the circulatory system, he, together with the vessels, goes to the thigh area through the obturator channel, located between the adductors. The nerve is associated with a group of adductor muscles, the knee and hip joints. Also, the nerve innervates the surface of the middle part of the thigh closer to the knee.
Of the entire lumbar plexus, the femoral branch is the largest. It originates at the border of the fifth vertebra of the lower back in the region of the same muscle fibers. Coming from the lateral edge of the muscle, the nerve goes lower between two other muscle groups: lumbar and iliac, going under the shell of the latter.
Going under the inguinal ligaments, the nerves of the lumbar plexus are divided into numerous branches that are associated with the skin and muscles of the front of the thigh, knee and hip joints.
Part of the whole
The nerve endings of the lower back are part of a common system called the "lumbosacral nerve plexus". The branches of the lumbar, sacral and coccygeal departments, interwoven with each other, form two main plexuses: the lumbar and sacral. With the first term, now everything is clear, we can move on to another definition.
Part of the anterior branch takes part in the formation of the sacral plexus (plexus sacralis), which comes from the fourth and fifth lumbar, as well as from the first through third sacral branches of the spinal nerve endings. The lumbar plexus itself is located in the pelvis directly on the connective tissue of the piriformis muscle. It is presented in the form of a thick plate of triangular shape, the apex of which is turned towards the sub-piriform slit.
The base of the triangle is near the pelvic openings. At the same time, some part of the plexus is located in front of the sacrum, and the other in front of the piriformis muscle. On all sides it is surrounded by loose connective tissue. As in the lumbar region, there is also a set of nerve endings, which can be either short or long.
Short nerves of the sacral region
Short branches are the following nerves:
- gluteal (upper and lower);
- sexual;
- internal locking;
- pear-shaped;
- nerve of the quadratus thigh muscle.
The gluteal nerves of the lumbosacral plexus are divided into upper and lower. The first pair with the gluteal artery leaves the pelvic cavity through the supra-piriform aperture. The nerve is connected with the small and medium gluteus maximus muscles, as well as with fibers connected to the broad fascia of the thigh. The lower nerve together with the artery leaves the pelvic region through the sub-piriform aperture and connects to the gluteus maximus muscle. But besides her, he is associated with a capsule of the hip joint.
Through the same pear-shaped opening, the pelvic cavity leaves the genital nerve, bypasses the sciatic bone from the back and goes straight to the sciatic-rectal fossa. Here it is divided into lower rectal and perineal branches. Moreover, the first are associated with the external sphincter of the anus and the skin of the anal region. The latter are responsible for the innervation of the muscles and skin of the perineum and scrotum of the male body. The female lumbosacral plexus is arranged a little differently. Anatomy is different in that the perineal branch is connected with the labia majora.
Long nerves of the sacral region
Long branches are represented by:
- posterior cutaneous nerve;
- sciatic nerve.
The posterior cutaneous nerve ending leaves the small pelvis along the sub-piriform aperture, descending not far from the sciatic nerve. The posterior femoral cutaneous nerve near the lower edge of the gluteus maximus muscle is divided into the lower gluteal and perineal nerve branches. In this case, the lower branch innervates the skin of the lower surface of the buttocks.
The posterior cutaneous femoral branch runs along the groove between the semi-tendon and biceps femoral muscles. Its branches penetrate the broad fascia of the thigh and are divided into smaller ones from the inner surface of the thigh, reaching the popliteal fossa.
The sciatic nerve ending, which is part of the sacral and lumbar plexus, is the largest branch in the human body and deserves special attention. By means of a sub-piriform aperture, the nerve leaves the pelvis together with other nerves (lower gluteal, genital, posterior cutaneous femoral) and the sciatic artery, heading downward. About the same line with the rhomboid depression, which is behind the knee joint, it is divided into two branches: the tibial and the common fibular.
Tibial branch
It is vertically directed down towards the soleus muscle of the ankle-popliteal canal. Throughout its length, this nerve is divided into numerous branches. Some of them approach the triceps muscle of the lower leg, others go to the long flexor muscle fibers of the fingers and big toe. There are those that are connected to the plantar and popliteal muscle.
The most sensitive endings included in the sacral and lumbar plexus are connected to the capsule of the knee joint, the interosseous membrane of the lower leg, the ankle joint, and the bones of the lower leg. The largest sensitive branch of the tibial branch is the medial cutaneous caviar nerve. It moves away from this branch and goes under the skin surface and intertwines with the cutaneous caviar nerve, which, in turn, comes from the common peroneal nerve.
The result of the fusion of these two endings is the formation of the calf nerve. First, it runs along the side of the ankle and then goes along the lateral edge of the foot. In this place, it is already called the lateral dorsal skin nerve, which is responsible for the innervation of the skin in these areas.
Common peroneal branch
It passes a little away from the neck of the fibula in the place where the popliteal fossa is located. Continuing to consider the lumbar plexus and its branches, it is worth noting that in this place the latter are divided into two main branches:
The superficial nerve is directed downward. His responsibilities include the innervation of the short and long peroneal muscles. Leaving this channel, the nerve goes to the rear side of the foot, where it is divided into medial and intermediate back skin endings.
The medial nerve provides sensitivity to the skin of the back of the foot near its lateral edge, as well as the back of the skin of 2 and 3 fingers. For the innervation of the back of the skin surface of the 3, 4 and 5 fingers meets the intermediate cutaneous nerve ending.
The deep nerve enters the opening of the anterior intermuscular septum of the lower leg and, accompanied by the artery of the same name, rushes down. At the level of the lower leg, the nerve is divided into several endings that connect the anterior tibial muscle and the long muscle of all toes. Approximately at the border of the first intertarsal space, this nerve has two back branches that innervate the skin surface of 1 and 2 fingers.
Pathological situations
One of the most common ailments is the defeat of the lumbosacral plexus, which is associated with pinching or pinching of the sciatic nerve. In this case, the largest nerve is compressed, which causes strong pain in the leg. Almost always, pathology occurs only on one side and rarely occurs in a bilateral form. The male half of humanity, which is associated with heavy physical work, is in a high-risk zone.
In medicine, this disease is referred to as sciatica, during the diagnosis it can be classified as sciatic nerve neuralgia or lumbosacral radiculitis. This name comes from the Greek word "ishia", which in translation means "seat." The sciatic nerve in Latin is called nervus ishiadicus.
Symptomatology
The main symptom, which indicates a defeat of the lumbar plexus, is severe pain in the buttocks and legs, which can occur in a different manifestation. Often, the pain is so severe that a person loses consciousness. In other cases, the pain may be burning, cutting, or stitching. Symptoms are also possible:
- In a standing position, it is impossible to lean on a sore leg, and when lying down you have to look for a comfortable position.
- The pain comes mainly at night, especially after working in cold weather.
- In some cases, the pathology first appears on the back of the thigh, and then reaches the lower leg and foot.
- If you stay in one position for a long time (lying, sitting), the pain intensifies, which also manifests itself with prolonged walking.
- Sneezing, coughing, laughing also provoke the onset of pain.
- After taking the appropriate drugs or after the subsiding of the attacks, the residual pain goes to the lower back.
Often, pinching of the root of the lumbosacral plexus is not in vain and can lead to impaired gait and cause sweating of the feet. You can also feel tingling or burning of the lower leg and foot. Often, due to the disease, the leg in the knee is almost impossible to bend. The same can be said for the toes and the foot, which cannot be turned.
Diagnostics
An obvious clinical picture, which the patient describes at the doctor’s appointment, will help determine the damage to the sciatic nerve. Any specialist will notice a change in the nature of tendon reflexes and sensitivity on the side that the patient complains about. Sometimes an initial examination does not allow an accurate diagnosis of the ailment to occur. In this case, it is necessary to conduct additional studies, among which are:
- X-ray
- computed tomography;
- MRI
- Ultrasound
- radioisotope scanning of the spine.
Thanks to computed tomography, which is a more accurate x-ray method, even minor changes in the spine can be detected.
But in some cases, when this study is contraindicated, the doctor prescribes MRI of the lumbosacral plexus.
Treatment
To get rid of the pathology, they resort to one of two methods of treatment - conservative or surgical. But they always start with the first technique, which includes a set of diverse activities. In acute sciatica, bed rest on a hard mattress with minimal motor activity and diet is recommended. You need to eat warm, not spicy, not smoked and not fried, mostly liquid foods (meat and vegetable soups and milk porridges).
Drug treatment involves taking medications prescribed by your doctor. As soon as the pain begins to recede, therapeutic exercises are indicated. All exercises are selected depending on the nature of the disease.