The sympathetic nerve trunk is one of the components of the nervous peripheral part of the sympathetic system.
Structure
In accordance with the structure of the sympathetic trunk (Truncus sympathicus), it is paired and is the nodes that are connected to each other through sympathetic fibers. These education data are located on the sides of the spinal column throughout its length.
Any of the nodes of the sympathetic trunk is a cluster of vegetative neurons that switch preganglionic fibers (most of them) that leave the spinal cord, forming connecting white branches.
The above fibers are in contact with the cells of the corresponding node or go as part of the inter-nodal branches into the lower- or higher-lying node of the sympathetic trunk.
Connective white branches are located in the upper lumbar and thoracic regions. In the sacral, lower lumbar and cervical nodes, branches of this type are absent.
In addition to white branches, connective gray branches are also distinguished, which consist mainly of sympathetic postganglionic fibers and connect the spinal nerves to the nodes of the trunk. Such branches go to each of the spinal nerves, departing from each of the nodes of the sympathetic trunk. As part of the nerves, they are directed to the innervated organs (glands, smooth and striated muscles).
In the sympathetic trunk (anatomy), the following departments are conventionally distinguished:
- Sacral.
- Lumbar.
- Thoracic.
- Cervical.
Functions
In accordance with the departments of the sympathetic trunk and its ganglia and nerves, several functions of this anatomical formation can be distinguished:
- The innervation of the neck and head, as well as control over the contraction of the vessels that feed them.
- Innervation of the organs of the chest cavity (branches from the nodes of the sympathetic trunk are part of the nerves in the pleura, diaphragm, pericardium and ligaments of the liver).
- Innervation of the vascular walls (as part of the nerve plexuses) of the common carotid, thyroid and subclavian arteries, as well as the aorta.
- Connect the nerve ganglia with the nerve plexuses.
- Participate in the formation of the celiac, aortic, superior mesenteric and renal plexuses.
- Innervation of the pelvic organs due to the entry of branches from the cruciate ganglia of the sympathetic trunk into the lower hypogastric plexus.
Cervical sympathetic trunk
The cervical spine contains three nodes: lower, middle and upper. We consider each of them in more detail below.
Upper knot
The formation of a fusiform shape with dimensions of 20 * 5 mm. It is located on 2-3 cervical vertebrae (their transverse processes) under the prevertebral fascia.
Seven main branches depart from the node that carry postganglionic fibers that innervate the organs of the neck and head:
- Connecting gray branches to 1, 2, 3 spinal cervical nerves.
- N. jugularis (jugular nerve) is divided into several branches, two of which are attached to the glossopharyngeal and vagus nerves, and one to the hyoid nerve.
- N. caroticus internus (inner carotid nerve) enters the outer shell of the internal carotid artery and forms the plexus of the same name, from which sympathetic fibers extend in the region of the artery into the canal of the same name on the temporal bone, which form a stony deep nerve passing through the pterygoid canal in the sphenoid bones. After exiting the canal, the fibers pass the pterygopalatine fossa and join the parasympathetic postganglionic nerves from the pterygopalatine node, as well as the maxillary nerve, and then go to the organs in the face area. In the carotid canal, branches are separated from the carotid internal plexus, which penetrate and form the plexus in the tympanic cavity. Inside the skull, the carotid (internal) plexus passes into the cavernous, and its fibers spread through the vessels of the brain, forming plexuses of the ocular, middle cerebral, and anterior cerebral arteries. In addition, the cavernous plexus gives off branches that connect with the parasympathetic fibers of the parasympathetic ciliary node and innervate the muscle that dilates the pupil.
- N. caroticus externus (carotid external nerve). It forms the external plexus near the artery of the same name and its branches, which supply blood to the organs of the neck, face and hard shell of the brain.
- The pharyngeal-laryngeal branches accompany the vessels of the pharyngeal wall and form the pharyngeal plexus.
- The cardiac superior nerve passes near the cervical region of the sympathetic trunk. In the chest cavity forms a superficial cardiac plexus, which is located under the aortic arch.
- Branches that are part of the phrenic nerve. Their endings are located in the capsule and ligaments of the liver, pericardium, parietal diaphragmatic peritoneum, diaphragm and pleura.
Middle node
The formation is 2 * 2 mm in size, located at the level of 4 cervical vertebrae, in the place where the common carotid and lower thyroid arteries intersect. This node gives rise to four types of branches:
- Connective gray branches that go to 5, 6 spinal nerves.
- The nerve is the average cardiac that is located behind the carotid common artery. In the chest cavity, the nerve is involved in the formation of the cardiac plexus (deep), which is located between the trachea and the aortic arch.
- The branches that participate in the organization of the nerve plexuses of the subclavian, common carotid and thyroid lower arteries.
- An interstitial branch that connects to the cervical superior sympathetic ganglion.
Bottom node
The formation is located behind the vertebral and above the subclavian arteries. In rare cases, it combines with the first sympathetic thoracic node and is then called the stellate (cervicothoracic) node. The bottom node gives rise to six branches:
- Connecting gray branches going to 7, 8 spinal cervical nerves.
- The branch leading to plexus vertebralis, spreading in the skull and forming the plexus of the cerebral posterior artery and the basilar plexus.
- The lower cardiac nerve that lies to the left behind the aorta, and to the right behind the brachiocephalic artery and participates in the formation of the deep cardiac plexus.
- The branches that enter the phrenic nerve, but do not form plexuses, but end in the diaphragm, pleura and pericardium.
- The branches that form the plexus of the carotid common artery.
- Branches to the subclavian artery.
Thoracic department
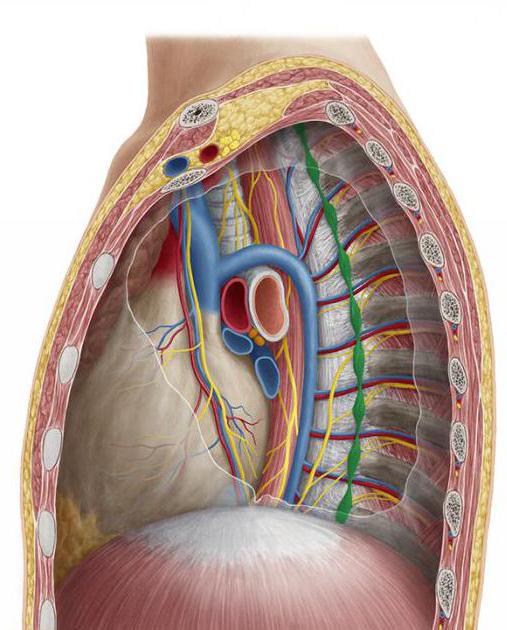
The composition of the thoracic sympathetic trunk includes ganglia thoracica (thoracic nodes) - nerve formations of a triangular shape that lie on the costal necks from the sides of the thoracic vertebrae, under the intrathoracic fascia and parietal pleura.
6 main groups of branches depart from the thoracic ganglia:
- The white connecting branches that branch off from the intercostal nerves (their anterior roots) and penetrate the nodes.
- The gray connecting branches emerge from the ganglia and are sent to the intercostal nerves.
- The branches of the mediastinum. They originate from 5 sympathetic superior gangias and pass into the site of the posterior mediastinum, together with other fibers, forming the bronchial and esophageal plexus.
- Cardiac pectoral nerves. They originate from 4-5 sympathetic superior ganglia, participating in the formation of the aortic and deep cardiac plexuses.
- The nerve is large internal. Collected from the branches of 5-9 sympathetic pectoral nodes and covered with intrathoracic fascia. Through the holes between the intermediate and medial legs of the diaphragm, this nerve passes into the abdominal cavity and ends in the ganglia of the celiac plexus. The structure of this nerve includes a large number of preganglionic fibers (which switch in the ganglia of the celiac plexus to postganglionic fibers), as well as postganglionic, which have already switched at the level of the thoracic ganglia of the sympathetic trunk.
- The nerve is small intranostal. It is formed by branches of 10-12 nodes. Through the diaphragm, it falls a little lateral n. splanchnicus major and also enters the celiac plexus. Part of the preganglionic fibers of this nerve in the sympathetic ganglia switch to postganglionic, and part follows to the organs.
Lumbar
The lumbar ganglia of the sympathetic trunk are nothing more than a continuation of the chain of ganglia of the thoracic region. The lumbar includes 4 nodes that are located on both sides of the spine on the inner edge of the large lumbar muscle. On the right side, the nodes are visualized outwards from the vena cava inferior, and to the left, outwards from the aorta.
The branches of the lumbar sympathetic trunk are:
- White connecting branches extending from 1 and 2 spinal lumbar nerves and suitable for 1 and 2 ganglia.
- Gray connecting branches. Combine the lumbar ganglia with all the spinal lumbar nerves.
- The internal lumbar branches that depart from all the ganglia and enter the superior hypogastric, celiac, aortic abdominal, renal and superior mesenteric plexuses.
Sacral department
The lowest section (respectively, of the topography of the sympathetic trunk) is the sacral section, which consists of one unpaired coccygeal ganglion and four paired sacral ganglia. The nodes are located a little medial to the sacral anterior openings.
There are several branches of the sacral section of the sympathetic trunk:
- Connecting gray branches directed to the sacral and spinal nerves.
- Internal nerves, which are part of the autonomic plexuses in the pelvis. Visceral fibers from these nerves form the hypogastric plexus, lying on the branches from the iliac internal artery, due to which the sympathetic nerves penetrate the pelvic organs.