Pathological processes affecting the intestine develop gradually and in the initial stages practically do not bother patients. That is why people often remain without adequate medical care until the disease becomes chronic. What symptoms indicate diseases and how to treat an intestinal infection, we will understand together.
Intestinal diseases are a group of inflammatory processes that occur in the colon and small intestine. As a result of various negative factors, damage and thinning of the mucous membrane lining the internal organs occurs. Gastroenterologists deal with intestinal problems.
Factors affecting the development of intestinal pathologies
Diseases of the stomach and intestines are caused by exposure to the body of negative factors, and in rare cases, one cause is the cause of inflammation. The more various factors simultaneously affect the human body, the more difficult the disease will be and, as a result, it will be harder to treat.
Factors affecting the development of any intestinal pathologies include:
- violation of diet;
- immunological disorders;
- mental stress and stressful situations;
- genetic factor;
- physical inactivity;
- intestinal viral infection;
- bacterial intestinal infection;
- alcohol abuse, smoking;
- taking certain medications (e.g. antibiotics).
Diseases of the small intestine include enteritis (a pathological violation of the functionality of the small intestine), carbohydrate intolerance, gluten enteropathy (occur due to the lack of necessary enzymes in the body), vascular and allergic diseases of the small intestine, Whipple's disease, and others. All of them begin their development due to a violation of the integrity or irritation of the mucous membrane lining the small intestine, due to improper nutrition or the use of specific medications.
Diseases of the large intestine include colitis, including ulcerative, Crohn's disease, diverticulosis and other irritations of the colon, tumors and other diseases. Most often, inflammatory processes in this area arise due to a bacterial infection, however, cases where the cause is a long course of antibiotics, malnutrition, etc.
Small bowel disease
When it comes to bowel disease, symptoms and treatment depend on the negative factors that triggered the pathology. The small intestine is the longest part of the gastrointestinal tract. It is involved in the absorption of nutrients from food. When considering diseases of the small intestine, it is necessary to take into account not only the factors of their appearance, but also their various combinations. This will allow the patient to appoint the most appropriate therapy.
Inflammatory processes that occur in the small intestine are called enteritis. The disease is usually acute or chronic. The cause of acute enteritis is usually an infection (food poisoning, “dirty hands disease”, etc.). The characteristic symptoms of diseases of the small intestine are expressed by the appearance of nausea, vomiting, diarrhea and other signs of general intoxication, as well as an increase in body temperature, fever. The causative agents are salmonella, cholera and other microorganisms of the typhoid parathyphoid group. For chronic enteritis, bacterial and protozoal infections, various disorders of the immune system are characteristic. A feature of the chronic form of enteritis is the fact that it is preceded by an inflammatory or inflammatory-dystrophic disorder occurring in the small intestine. As a result of such a violation, a person develops digestive problems, the reproduction of pathogens in the small intestine occurs, which leads to immune and metabolic problems.
Symptoms of small bowel disease
In bowel disease, symptoms and treatment depend on the severity of the inflammation and its location. Signs of the disease can range from mild to severe. The periods of the active phase of the disease are replaced by periods of remission. The clinical picture of inflammation of the small intestine is characterized by the following manifestations:
- diarrhea - is a common problem for people with similar diseases;
- increased body temperature and increased feeling of fatigue - often with problems with the intestines a person has a low-grade fever, he feels exhausted and broken;
- abdominal pain, colic - inflammation and ulceration of the mucous membrane of the small intestine can affect the normal movement of food through the gastrointestinal tract and thereby cause pain and cramping;
- nausea, vomiting;
- the presence of blood in the stool - usually it indicates internal bleeding of the small intestine;
- decreased appetite - abdominal pain and colic, as well as the presence of an inflammatory process in the body, as a rule, dulls a feeling of hunger;
- rapid weight loss.
The clinic of chronic diseases of the small intestine is caused by the development of recurring diarrhea and malabsorption syndrome. Diarrhea is provoked by hypersecretion of water and calcium ions in the body, intestinal hyperexudation, increased osmotic pressure and impaired transport function of the intestinal contents. Impaired absorption syndrome is a consequence of recurrent diarrhea.
Symptoms of the chronic form of the disease include enteric dispersion syndrome (the appearance of discomfort in the abdomen in the area around the navel). In addition, the patient is tormented by rumbling and a bursting feeling in the lower abdomen, bloating. Abdominal pain can be spastic, cramping, or dull. If the pain intensifies after eating, this means that the disease has passed into a neglected form.
Colon diseases
Diseases of the colon include chronic inflammation of all or parts of the colon. First of all, it is ulcerative colitis and Crohn's disease. Both diseases are associated with severe diarrhea, excruciating abdominal pain, fatigue, and weight loss. If a person has a suspicion of bowel disease, symptoms and treatment should be identified as soon as possible, since the lack of adequate therapy can lead to life-threatening complications.
Ulcerative colitis is an inflammatory disease that causes ulcers to form on the inner wall of the colon. Crohn's disease is characterized by inflammation of the mucous membrane of the entire gastrointestinal tract, inflammation usually spreads deep into the affected tissues and can affect both the large and small intestines. Collagen and lymphocytic colitis are also considered diseases of the colon, but, as a rule, are considered separately from the classic inflammatory bowel diseases.

The exact causes of inflammatory bowel disease are still unknown. Earlier, pathological factors included stress, abuse of diets. Now doctors know that such causes can aggravate, but not provoke, a problem. It is believed that most often diseases of the large intestine arise as a result of a bacterial infection that penetrates into it with poor-quality food, drinks, and the use of antibacterial drugs. Also one of the possible reasons is a violation of the immune system and heredity. Problems with the intestines also appear due to narrowing of blood vessels in the colon and a violation of its blood supply. As a rule, this reason is typical for the elderly.
Symptoms of the colon
Many signs of bowel disease are typical and overlap. Characteristic symptoms include abdominal pain of a dull or cramping nature, possibly cramping. The inside of the colon is covered with ulcers that can bleed. Patients complain of morning fatigue, defecation with the release of blood and mucus, anemia (with the loss of a large amount of blood), joint pain. Often with the disease, uncontrolled weight loss, loss of appetite, fever, flatulence, dehydration occur. Often the patient has anal fissures.
It is very important that such a disease of the large intestine, the symptoms of which can be mistaken for other diseases, is diagnosed in a timely manner. In the absence of adequate treatment, the patient has increased risks to the development of complications (oncology, fistulas, intestinal ruptures and intestinal obstruction).
Chronic enterocolitis
Chronic enterocolitis is a simultaneous inflammation of both the small and large intestines, which is characterized by atrophy of the mucous membrane lining the inner surface of the intestines, which causes a violation of intestinal functions. Depending on the location of the inflammatory process, the disease is classified separately for small (enteritis) and large (colitis) intestines.
The causes of chronic enterocolitis are due to the impact on the human body of the following pathological factors:
- prolonged malnutrition;
- violation of immunity and metabolism;
- hormonal disorders, stress;
- intoxication with drugs and chemicals;
- structural features of the intestine;
- intestinal viral infection;
- diseases of internal organs;
- intestinal and parasitic infections.
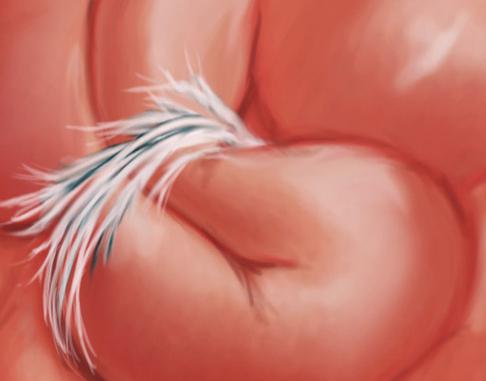
One of the most common pathogens of chronic enterocolitis is intestinal giardia (a photo of these parasites can be considered in the article). They are able to multiply rapidly and cause giardiasis. Signs of the disease include diarrhea, excess gas, cramping and abdominal pain, nausea, and vomiting. Giardia, the photo of which is presented in the picture, exists in two forms: active and inactive. Active forms of parasites live in the human body, when they go outside, together with feces, they become inactive and spread the infection outside the body.
Chronic enterocolitis is often the result of untimely or poor-quality treatment of acute forms of inflammatory bowel processes. In addition, there is a risk of transmission of the disease by inheritance and in people who were breastfed in infancy.
Adhesive bowel disease
Adhesions are thin fibrous tissues that form in the abdominal cavity due to various negative factors. Adhesive bowel disease, the symptoms of which are often expressed in the appearance of spasmodic pain, is especially dangerous for humans. The main complaint of patients, as a rule, is chronic abdominal pain, the nature of which is difficult to determine. Sometimes there is intestinal obstruction, constipation, disorders. In addition, adhesive bowel disease, the symptoms of which can be similar to gynecological problems, often causes female infertility.
The main symptoms of the disease include discomfort in the navel, cramps, and a feeling of fullness in the abdomen. In places where adhesions appear, intestinal twisting occurs, which interferes with the normal movement of its contents. Perhaps the development of complete intestinal obstruction. Unfortunately, not many diagnostic methods are able to detect adhesions: they are not visible both on the x-ray and ultrasound. They can be considered when using barium contrast for computed tomography. Adhesive disease is treated with laparoscopic surgery or with open surgery by dissecting the adhesions with a scalpel or electric current.
Diagnosis of intestinal diseases
Diagnosis of inflammatory bowel disease should only be after the exclusion of other possible problems. This will require a combination of diagnostic tests. Diagnosis of intestinal diseases includes the following tests and procedures:
- Blood test - it is necessary to control hemoglobin levels.
- Analysis of feces for the detection of blood in it.
- Colonoscopy - allows you to view the entire rectum using a thin flexible tube with a camera connected to it. During the procedure, the doctor may take tissue samples for additional analysis (biopsy).
- Flexible sigmoidoscopy - performed using a thin flexible tube with a light sensor that allows you to examine the sigmoid portion of the colon.
- Upper endoscopy - the doctor uses a thin, flexible, lighted tube to examine the esophagus, stomach and first part of the small intestine.
- Capsular endoscopy - performed to diagnose Crohn's disease.
- X-ray diagnostics - necessary for serious problems with the intestines, in order to exclude serious complications (for example, perforation of the colon).
- Computed tomography - the method allows you to consider more different details in the image than with x-rays. The test evaluates the entire intestine, as well as the tissue outside it.
- Magnetic resonance imaging - is a particularly effective method for eliminating fistulas, tears and other complications.
Bowel Disease Treatment
To effectively heal bowel disease, symptoms and treatment must be closely linked. The goal of treating inflammatory bowel diseases is to reduce the inflammatory process that causes symptoms and causes discomfort. Adequate therapy will not only facilitate the manifestation of the disease, but also lead to prolonged remission, reduce the risks of complications. Before treating an intestinal infection, the doctor conducts a thorough diagnosis, which will allow you to choose the most effective methods of therapy.
Treatment can be carried out with medical, folk and surgical methods. Medications can relieve symptoms and reduce the risk of complications. It should immediately be said that many patients will be forced to take medication for a long period of time. The choice of drugs depends on the localization of inflammation, the severity of the symptoms of the disease and will be aimed at preventing relapse of the disease. Sometimes it may be necessary to combine drugs, supplement drug therapy with alternative recipes.
The following categories of drugs are used to treat intestinal infections and inflammatory processes:
- anti-inflammatory drugs (aminosalicytals, corticosteroids);
- antibacterial drugs (for example, Ciprofloxacin);
- immunomodulators (drugs "Methotrexate", "Azathioprine");
- disease-modifying agents (drugs "Infliximab", "Adalimumab").
Drug treatment should be accompanied by changes in the diet, stress reduction, compliance with the rest regimen. A very important stage of treatment is to ensure that patients have a diet for bowel disease. The diet should consist of healthy, balanced foods with enough protein and nutrients. The diet is selected individually for each individual patient. The general recommendations regarding proper nutrition include the following:
- eat small meals throughout the day;
- drink plenty of clean water (up to 2 liters in small portions, evenly distributed throughout the day);
- Avoid foods high in fiber (legumes, nuts, bran);
- abandon fatty and fried foods, sauces, foods that cause bloating;
- limit dairy products (with lactose intolerance);
- during treatment it is important to take vitamins B12, D, calcium, iron preparations.
Often the treatment of intestinal diseases is carried out surgically. The main operations, referred to as resections, include the removal of the affected intestinal tract. Treatment of abscesses and fistulas in the anus is carried out with the help of surgical intervention followed by drainage.
Prevention
Proper digestive function begins with good overall health. The organs of the gastrointestinal tract depend on a reliable immune system, which is able to withstand infectious factors. Preventive measures are aimed at improving the human health and well-being.
- To give up smoking. , , , . , 30% , , , 40% – . , , .
- Body weight control. , , , .
- Active lifestyle. , - , .
- Balanced diet. . , .