An inflammatory lesion of the central nervous system, which is presumably of an autoimmune nature, is called acute disseminated encephalomyelitis. It manifests itself as a complication of a recent infectious disease or may develop due to immunization. Treatment of the disease occurs under the supervision of a physician.
The concept of pathology
Acute disseminated encephalomyelitis is a rather dangerous ailment in which the brain and spinal cord are affected. With untimely treatment and in complex cases, a fatal outcome is possible.
It is believed that children are most susceptible to pathology. The average age at which the disease is noted in this category of people is 8 years. It can begin in infancy (3 months), and most often occurs up to 10 years. In adulthood and old age, the disease begins, respectively, at 33.9 and 62.3 years.
Primary and secondary forms of the disease are distinguished. At the first, it appears as a result of the action of a viral infection. Secondary acute encephalomyelitis develops as a result of complications after various ailments of a viral nature or after vaccination.
Classification
In the area that is affected by the disease, the following types of encephalomyelitis are distinguished:
- Disseminated myelitis. In this case, the spinal cord is disrupted.
- Opticomyelitis and optoencephalomyelitis. They are characterized by a similar pathogenesis, while there are lesions of both the brain and spinal cord, as well as damage to the optic nerves.
- Polyencephalomyelitis. With this disease, the work of the nuclei of the nerves of the skull located in the brain stem is disrupted, the spinal cord (its gray matter) is also affected.
- Encephalomyelopoliradiculoneuritis. One of the most common such pathologies. In this case, violations of almost all components of the nervous system are observed.
The most commonly diagnosed acute disseminated encephalomyelitis. With this disease, various parts of the brain and spinal cord are affected. Pregnancy in acute disseminated encephalomyelitis proceeds as usual.
There is no unified classification of this disease. In general, the following varieties are distinguished:
- stem encephalitis;
- cerebellitis;
- opticomyelitis;
- optic neuritis;
- acute transverse myelitis;
- acute hemorrhagic leukoencephalitis.
In the first variety, the following symptoms are observed:
- violation of respiratory acts;
- facial nerve neuritis;
- violation of the swallowing process.
At present, myalgic encephalomyelitis is also isolated. It develops after vaccination or an ailment of a viral origin. In this case, the following symptoms appear:
- muscle pain;
- violations of the digestive tract;
- frequent mood swings;
- depression;
- the appearance of pain in the articular areas;
- fatigue after small loads;
- chronic fatigue.
Causes
To date, they are not fully understood. It is still unknown why the body begins to produce proteins aimed at combating the nervous system.
The progression of the disease is noted in the following of them:
- colds;
- allergy;
- decrease in body reactivity ;
- the introduction of certain types of vaccines;
- viral infections, especially those that cause various skin rashes: rubella, chickenpox, herpes;
- traumatic brain injuries.
Signs
The disease begins rapidly. Symptoms of acute disseminated encephalomyelitis are divided into cerebral and focal. The first include the following:
- decreased intelligence;
- memory impairment;
- impaired consciousness;
- epilepsy attacks.
In their absence, the diagnosis of acute disseminated encephalomyelitis is doubtful.
Focal symptoms manifest as multiple brain lesions. They are mainly combined in the form of the following:
- oculomotor disturbances;
- extrapyramidal;
- cerebellar;
- pyramidal.
Only by these signs can a correct diagnosis be made only by a highly qualified doctor.
The two categories of symptoms of acute disseminated encephalomyelitis described above appear for 7-14 days, after which the clinical picture becomes less pronounced. Against the background of the ongoing disease, disturbances in the peripheral nervous system may appear. A condition such as polyneuropathy may appear.
Different symptoms may occur depending on which part of the brain is affected.
Initial signs may appear already during an infectious disease that causes encephalomyelitis, with asthenia and an increase in body temperature. These include:
- tingling sensation in the legs - is quite rare;
- violations in the digestive tract;
- increased arousal, sometimes replacing lethargy;
- runny nose, sore throat;
- drowsiness;
- possible increase in body temperature, although not necessary;
- headache;
- general malaise.
If the brain is affected, then the following signs of the disease can be observed:
- the occurrence of a convulsive syndrome similar to an epileptic seizure;
- paresis of limbs;
- paralysis;
- speech impairment.
With damage to the roots of the spinal cord, the following symptoms are observed:
- pain syndrome that spreads along the spinal column, resembling the clinical manifestations of lumbago;
- the functioning of the pelvic organs worsens: urinary retention, bowel movement, or the reverse pattern of incontinence may occur;
- pain and temperature sensitivity of the body decreases;
- trophic changes in the epidermis appear.
With damage to the optic nerve, the following symptoms are observed:
- there is pain in the orbit, which gradually increases, especially when committing sudden movements by the organs of vision;
- a “veil” forms before the eyes;
- vision deteriorates.
The main differences between acute multiple encephalomyelitis and multiple sclerosis are as follows:
- unlike the latter, autoimmune reactions to myelin antigens do not have a chronic course and are limited to one exacerbation;
- the structure of the foci in both diseases is the same, however, the inflammatory dynamics and edema are more pronounced with the disease in question, oligodendrocytes are less affected.
Diagnostics
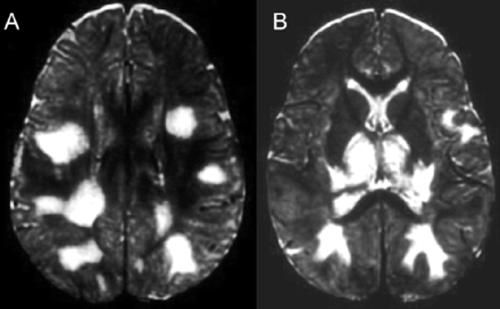
To detect the disease, an MRI scan is used for acute disseminated encephalomyelitis using contrast. Features of the disease are easily detected by the doctor in the picture or screen. In the FLAIR and T2 modes, asymmetric hyperintensive foci are defined that have poor outlines in both the white and gray matter of the brain, and in the second they may not be expressed. They can be small (up to 0.5 cm), large (more than 2 cm) and medium (having intermediate values). Sometimes large drainage foci with perifocal edema are noted, which cause a displacement of the surrounding structures. Optic tubercles may also be involved. In large areas of inflammation, hemorrhages are observed. Contrast material in the foci accumulates with different intensities. They can be detected in the spinal cord in a small number of cases, not exceeding 30%. After identifying the disease and conducting its treatment, patients are recommended to have an MRI scan again after six months. A decrease in demyelination sites or their complete disappearance indicates the correct diagnosis and the exclusion of multiple sclerosis.
In addition, the diagnosis, if necessary, can be performed using lumbar puncture. In this case, the patient is laid on his side with the implementation of local anesthesia. A needle is inserted between the lumbar vertebrae to collect a small amount of cerebrospinal fluid, which is analyzed. If there is a disease, a large number of lymphocytes will be found in it.
Additionally, perimetry, ophthalmoscopy, oculist consultation can be prescribed.
Be sure to make a diagnosis should take into account the presence in the clinical picture of signs of cerebral syndrome or encephalopathy. The latter includes patient complaints of nausea, vomiting, headaches, and there are disturbances in behavior and consciousness - from stupidity and drowsiness to the development of coma of varying degrees.
Variants of the course of the disease
Currently, there are three such:
- monophasic;
- returnable;
- multiphase.
In the first case, a single episode of a neurological disorder occurs and then the resolution of the disease occurs.
With the return option, the same symptoms are noted or even their increase 3 months after the start of the first attack or 30 days after the end of corticosteroid administration.
The multiphase course is characterized by the fact that after the same period of time new complaints and symptoms appear.
The goals of therapeutic treatment
The patient must first know that acute disseminated encephalomyelitis is treatable. But in order to achieve this, it is necessary to carry out appropriate treatment, which should be aimed at:
- detection and treatment of infections, which prevents its transformation into multiple sclerosis, every six months you need to check for their presence, making control immunograms;
- monitoring the body's immune state to select the optimal antiviral therapy;
- the maximum possible restoration of the work of brain areas affected by inflammation by stimulating remyelination;
- elimination of aggressive behavior of immunity to the central nervous system with normalization of the response of the first to the ingress of foreign microorganisms into the body.
Encephalomyelitis Treatment
Basic therapy is carried out with anti-inflammatory steroid drugs. Medium or high doses of Prednisone may be used depending on the patient’s condition, with a gradual decrease.
Corticosteroid therapy is carried out for 2-5 weeks. To prevent side effects, intravenous administration of immunoglobulins is prescribed. Remove immune antibodies and immune complexes from the body using plasmapheresis, which is carried out in complex cases.
Treatment of acute disseminated encephalomyelitis is aimed at eliminating the causes of the disease. For this, antiviral agents are assigned, belonging to the group of interferons.
Sometimes with a bacterial etiology of the disease, antibiotics can be prescribed:
- Kefzol;
- Gentamicin;
- Ampioks.
For the treatment of acute disseminated encephalomyelitis, accompanied by rheumatism, bicillin therapy is prescribed.
Symptomatic therapy is mandatory. Hemodynamics restoration, mechanical ventilation, resuscitation measures can be carried out.
To prevent cerebral edema, the following drugs are administered:
- "Furosemide";
- "Magnesia";
- "Diacarb."
How to eat with a diagnosis of acute disseminated encephalomyelitis? Severe dysphagia should be accompanied by nutrition through a probe.
When urine is retained, a catheter is inserted into the bladder. If intestinal paresis is observed, then enemas are done. In the presence of seizures, anticonvulsants are prescribed.
For the treatment of neurological disorders, anticholinesterase agents are prescribed: Proserin, Galantamine, B and C vitamins.
With convalescence, absorbable preparations are used: Cerebrolysin, Lidazu.
Treatment of disseminated encephalomyelitis may be accompanied by the use of nootropic drugs:
- Nootropil;
- "Ginkgo biloba".
Also, doctors can prescribe neuroprotectors: Mexidol, Semax.
Movement activity is restored by exercise therapy and massage. Transcranial magnetic stimulation is also performed.
With an exacerbation of the disease, treatment is carried out in a hospital. In this case, potent drugs are prescribed.
Folk remedies
They can be used, but not during exacerbation. They are mainly used at the recovery stage in order to maintain the functioning of the nervous system. The following recipes are used:
- The muzzle is spherical. Take 3 tbsp. l fruits, 250 ml of boiling water are poured, placed in a thermos, in which they are infused for 12 hours. The resulting infusion is drunk during the day in small portions. The treatment is carried out within two months.
- Mummy. 5 g is dissolved in 100 ml of water. Take three times a day for 1 tsp. 1 hour before meals three times a day.
- Onion with honey. The bulb is peeled and chopped with a grater. Squeezed juice, after which it is mixed with honey. Used three times a day for 1 tsp. for a month.
The main treatment method they should not be. Used with the permission of the attending physician.
The main differences in the course of the disease in children and adults
Previous vaccination or an infectious disease has most often caused acute disseminated encephalomyelitis in children. At the beginning of the development of the disease, they often have a fever, which is absent in adults. Children are characterized by a severe form of encephalopathy syndrome. In adults, it manifests itself in mild or moderate form with the possible appearance of hallucinations and delirium.
In children, signs of meningoencephalitis with the occurrence of ataxia are often observed; adults have motor and sensory deficits, radicular syndrome may be observed.
When conducting MRI foci in children are located in the spinal cord, trunk, cerebellum, cortex and the area of the basal nuclei, periventicular foci are rare. In adults, the latter are often observed, there is an increase in protein, pleocytosis.
Children recover quickly enough. At the same time, adults have a long hospitalization period with the same recovery.
Mortality in children is in the region of 5%, in adults - in the region of 8-25%. In small patients, the most favorable outcome of the disease. Gross residual deficiency is often characteristic of adults.
The consequences of acute disseminated encephalomyelitis
The disease can be characterized by a severe course, resulting in the formation of bulbar disorders, which can lead to death.
In the form of the consequences of acute disseminated encephalomyelitis, residual neurological deficiency can occur, leading to deep disability. Age-related changes are a risk factor for repeated exacerbations and the transformation of the disease into multiple sclerosis.
Some patients acquire persistent symptoms, manifested in the form of sensory disorders, visual impairment and paresis.
Prevention
To prevent the development of the disease, it is necessary to adhere to fairly simple rules:
- avoid physical overload during the course of the disease;
- give up bad habits and vaccinations;
- avoid overheating and overcooling of the body during the vaccination period.
Forecast
The acute period of the disease occurs within 1.5-2 weeks. In most cases, the prognosis is favorable. Up to 90% of patients undergo a monophasic course. In the majority of patients (70-90%), symptoms are subject to regression within six months after the onset of the disease, which is associated with remyelination processes.
The prognosis worsens with return and multiphase flow patterns. In this case, the acute form of the disease becomes chronic, and multiple sclerosis begins to develop.
Finally
Acute disseminated encephalomyelitis is characterized by impaired activity of the spinal cord and brain. In this case, patients may experience different symptoms depending on the affected departments and age. Diagnosis mainly involves an MRI of these organs. Treatment during an exacerbation is carried out in a hospital, includes the use of corticosteroids and, depending on the accompanying ailments, other means. By agreement with the doctor, phytotherapy can be used to restore the complex. A more favorable prognosis is for the monophasic variant of the course of the disease and for children, although in adults with a timely detected ailment and proper treatment, the prognosis is good.