The inflammatory process of the biliary tract caused by non-specific pathogens is called cholangitis. This is a fairly common ailment, and depending on the pathological changes that occur in the walls of the bile ducts, cholangitis is distinguished: purulent, necrotic, catarrhal and diphtheria. This article will focus on the purulent form of the disease.
general information
Previously, cholangitis was mainly diagnosed in the older age category, and in recent decades it has been increasingly detected in forty-year-old individuals. Mostly women suffer from this pathology. The disease usually proceeds against the background of other gastrointestinal anomalies - gastro- and duodenitis, gallstone disease, gastritis, hepatitis, cholecystitis, pancreatitis. In this regard, the course of the disease is quite severe. In addition, concomitant diseases create an obstacle to the effective prompt elimination of the cause of the disease. The acute purulent process of inflammation in the biliary tract, which is formed against a background of poor outflow of bile due to complete or partial blockage, leads to a purulent form of cholangitis.

The following clinic is characteristic of the disease: jaundice, which is rapidly growing, pain in the right side under the ribs, high fever, a feeling of cold. One of the complications of the disease is a combination of systemic inflammatory reactions to the process in the biliary tract with impaired consciousness, hemodynamics, the work of the kidneys and other organs. Diagnosis is by visualizing a mechanical obstruction revealed by CT or ultrasound of the abdominal cavity. Decompression of the biliary tract with the elimination of obstruction is carried out by surgery, after which antibiotic therapy is prescribed. Further adjustments are subject to other violations.
Reasons for the development of pathology
Purulent cholangitis is bacterial in nature. It is characterized by the presence on the walls of the bile ducts of wounds that after some time fester. This is a serious surgical pathology, which, without treatment, leads to the death of the individual. About half of all patients with this diagnosis have a purulent inflammatory process in the duct system.
Blockage of the bile duct with stones of dense formation is the main cause of purulent cholangitis. Other factors leading to failure of the outflow of bile and causing inflammation include:
- narrowing of the ducts after an injury;
- cicatricial changes;
- parasitic infestation;
- neoplasms in the region of the large papilla of the duodenum.
Pathogenic bacteria actively multiply in the biliary tract as a result of the cessation or incomplete outflow of bile. A small number of microbes are present in bile, having got into it from the jejunum hematogenously or with duodenobiliary reflux. With a normal outflow, inflammation does not develop, and the microflora maintains the immune system in good shape. If this process fails, the number of microorganisms in bile increases. Gram-negative microbes provoke the development of purulent cholangitis, in rare cases streptococci, staphylococci, pseudomonas.
The increase in internal pressure in the ducts of the liver leads to the fact that the bile contained in them, due to changes in resistance, will enter the bloodstream. As a result, bacteremia is observed. Most often, Klebsiella or Escherichia coli is detected. The leakage of pathogens into the blood flow system provokes the occurrence of biliary septic shock. In addition, the development of sepsis occurs as a result of endotoxemia. The endotoxins of bacteria, endowed with a pyrogenic effect, stimulate the blood coagulation system, which provokes the intravascular formation of clots. As a result of a humoral immune response, the kidneys fail. In the development of toxemia, a special role is played by impaired functioning of both general and local intestinal immunity.
Other causes of the disease
After removal of the gallbladder, cholangitis develops in more than fifty percent of cases. In this case, the disease is accompanied by severe inflammation of the ducts. The following factors provoke pathology:
- lesions by worms of the bile duct;
- hepatitis;
- postcholecystectomy syndrome;
- the penetration of pathogenic microorganisms from the intestine into the digestive tract;
- untreated cholecystitis;
- cysts on the bile ducts.
Clinical picture
With partial or complete obstruction of the bile ducts, acute purulent cholangitis develops. Everything happens suddenly and begins with a rise in temperature to forty degrees, chills, nausea, a feeling of fullness and heaviness in the right hypochondrium. Jaundice in this case manifests itself quite quickly. With an obstructive purulent form, yellowness of the sky, dermis and sclera is absent or appears later.

The classic triad of the acute course of the disease, namely pain syndrome, fever, jaundice, with complete obstruction of the bile ducts is observed in fifty percent of individuals. Biliary sepsis is always present - this term is used both in gastroenterology and in abdominal surgery to describe a very serious condition of an individual. With acute signs of stagnation of bile, sepsis develops within a few hours. Moreover, it can occur at lightning speed and be accompanied by multiple organ failure and multiple liver abscesses. The main signs of biliary sepsis are oliguria, impaired consciousness and low blood pressure.
Diagnostic measures
Initially, the physician assesses the history and complaints of the individual. If bile duct inflammation is suspected, the patient is consulted by an abdominal surgeon. He makes a preliminary diagnosis. The following symptoms indicate the development of biliary sepsis: yellowness, fever and pressure, an increase in pain syndrome, tachypnea, heart rhythm disturbance. In this case, the patient’s body does not respond to the intravenous administration of 500 ml of saline, there is a confirmed bacteremia, there is a thick pus in the bile ducts. Signs of acute inflammation are detected on the basis of laboratory tests:
- In the general clinical analysis of blood - an increase in the sedimentation rate of red blood cells, neutrophilic leukocytosis.
- In liver samples - hyperphosphatemia, hyperbilirubinemia, high cholesterol. In some cases, transaminase activity increases.
To diagnose purulent cholangitis, an ultrasound of the abdominal cavity organs is certainly carried out. Using this type of hardware research:
- identify the basis that caused the ailment;
- visualize the mechanical barrier and the expansion of the bile ducts above the level of the obstacle;
- detect parenchyma modifications in the case of the formation of a purulent-inflammatory process in the liver.
On CT, the results obtained are verified and confirmed. In addition, esophagogastroduodenoscopy is performed. If necessary, that is, if the doctor does not have complete information, then endoscopic retrograde cholangiopancreatography is recommended . If it is not possible to do it, use percutaneous transhepatic cholangiography.
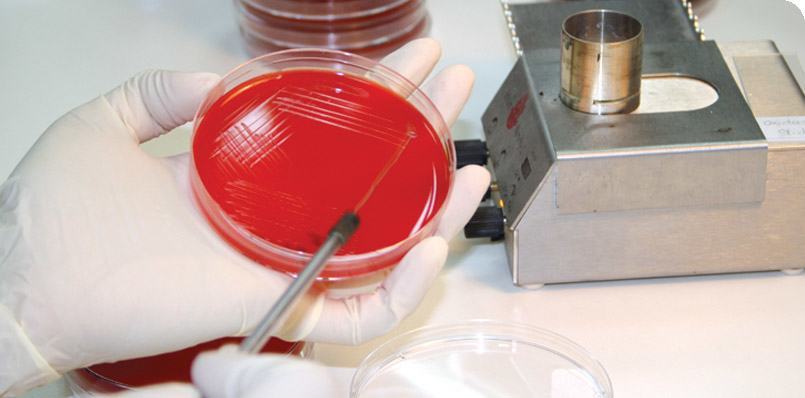
The contents of bile ducts obtained during the study are sent for bacteriological analysis, where the sensitivity of the pathogenic microorganism to antibiotics is determined. Bile is evaluated by a technician visually. The purulent form of the disease is proved by the presence of pus in it.
Surgical methods
Treatment of cholangitis, the symptoms of the purulent form of which were described above, requires immediate medical attention. When biliary sepsis has developed, emergency decompression of the biliary tract is necessary. If the cause of the pathology is cicatricial changes, then due to the installation of an endoprosthesis in the common bile duct, adequate compression is achieved.
Due to the fact that open surgeries are traumatic for patients and have frequent complications, nowadays doctors prefer minimally invasive interventions:
- Percutaneous transhepatic cholangiostomy is the final treatment in the presence of severe comorbidity. In other cases, this is preoperative preparation, during which bile is removed until the surgical elimination of interference.
- Mechanical lithotripsy.
- Endoscopic papillosphincterotomy - completely removes stasis of bile and obstructive jaundice. It is used in the etiology of calcululo-inflammatory nature.
- and some others.
Depending on the signs of stagnation of bile, the stage of violation of its outflow, the level of mechanical obstruction, the choice of method is assigned. After emergency decompression, radical treatment is performed - cholecystectomy, cholangioioduodenostomy or recanalization if the purulent form is caused by cicatricial narrowing of the biliodigestive anastomosis.
Conservative treatment
After urgent decompression, antibiotic therapy is indicated, it plays a supporting role. Difficulties at this stage of healing are associated with the fact that the identification of a pathogenic microorganism takes a long period, and in addition, after external drainage, the composition of the flora changes.
In practice, antibiotics are recommended to treat the symptoms of cholangitis before the results of the bacteriological study are ready. This is necessary to prevent bacteremia and sepsis. Initially, ureidopenicillins and cephalosporins are used in combination with Metronidazole. Some doctors recommend tetracyclines, penicillins, aminoglycosides.
An important stage of treatment is detoxification, since one of the severe manifestations is endotoxemia with purulent cholangitis. The drug "Polymyxin B is an endotoxin-binding drug, which is definitely recommended for use. It reduces the plasma concentration of Lactulose lipopolysaccharide, which is highly effective. In addition, the use of plasmophoresis allows the removal of plasma cytokines, endotoxins and circulating immune complexes. Using enterosorption, toxins are removed from the gastrointestinal tract, preventing them from entering the portal bloodstream. As well as immunocorrection and nutritional support.
Forecast
Purulent cholangitis or an inflammatory process that affects the biliary tract due to a malfunction or complete blockage of the outflow of bile is considered a severe surgical abnormality. The prognosis for this ailment is determined not only by the level of blockage of the biliary tract, but also by the timeliness of special special care. Unfortunately, mortality in this disease is quite high. The danger of a purulent form of the disease is that the clinic is similar to other varieties of this pathology, and untimely and incorrect treatment leads to very serious consequences - purulent intoxication, liver failure, the formation of abscesses in the liver.
Prevention
Serious complications can be avoided with endoscopic treatment of gallstone disease. In addition, the latest surgical equipment and the high qualification of an abdominal surgeon contribute to this. Individuals undergoing surgical treatment of purulent cholangitis, as well as patients who have a history of episodes of obstructive jaundice, are under the supervision of a gastroenterologist. For them, routine examinations are carried out, which are aimed at identifying the presence of calculi and cicatricial strictures of the biliary tract. They adhere to dietary nutrition throughout life. It helps to avoid disorders of the excretion of bile and bile formation. If necessary, take medications recommended by a doctor.
Abdominal surgeon: who is it and what is it treating?
This is a doctor who performs surgical interventions using various innovative techniques and diagnostic equipment. He operates:
- industrial and domestic injuries;
- inflammation of the appendix of the cecum;
- polyps, varicose veins of the peritoneal organs;
- penetrating wounds;
- neoplasms;
- hereditary and acquired diseases of the abdominal organs;
- retroperitoneal space.
In addition, it treats pancreatitis, cholelithiasis, ulcerative lesions, and is also involved in the prevention of complications and the rehabilitation of individuals.
In modern conditions, abdominal surgeons perform urgent and planned complex operations:
- At a distance (video surgery) - when the patient is in an inaccessible area, the doctor directs the actions of doctors through video communication.
- Organ and tissue transplantation.
- Minimally invasive endoscopic surgery (laparoscopy). In these cases, the surgeon is located outside the surgical field and, with the help of 3D images on the screen of the monitor and the robot, operates with the highest accuracy.
With all surgical interventions, doctors use robotic equipment and sophisticated diagnostic equipment. In multidisciplinary healthcare institutions, there are narrow specializations of abdominal surgeons - pediatric, hepatologist, oncologist, gastroenterologist, coloproctologist.
Now you know who the abdominal surgeon is and what heals.