Pulmonary embolism is a severe form of damage to the pulmonary circulation. It develops due to embolization of the branches of the pulmonary artery with a gas bubble or bone marrow, amniotic fluid, thrombus. And pulmonary embolism (pulmonary embolism) is the most common type of obstruction (more than 60%) of the arteries of the pulmonary circulation, although against the background of other cardiovascular diseases it has a low frequency (about 1 case per 1000 people). But the high mortality to primary medical contact and the complexity in the diagnosis and treatment make this disease extremely dangerous for the patient.
What is TELA
Thromboembolism is a blockage of the lumen of a blood vessel by a blood clot, thrombus. And in the case of pulmonary embolism, the clinic, the diagnosis and treatment of which will be discussed in the publication, this blockage occurs in the arteries of the pulmonary circulation. A blood clot enters the pulmonary artery through veins from a large circle of blood circulation. In 95-98% of massive pulmonary embolism, a large blood clot forms in the veins of the legs or pelvis, and only 2-3% - in the veins of the upper half of the body and in the jugular vein pool. In the case of recurrent pulmonary embolism, many small blood clots form in the cavities of the heart. Most often this happens with atrial fibrillation or with thromboendocarditis of the right heart.
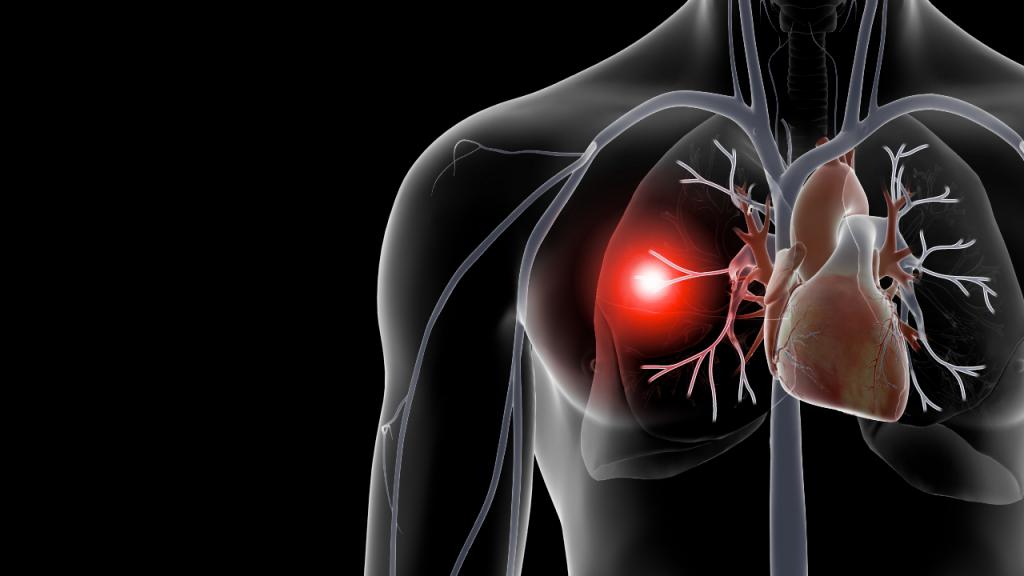
Pulmonary thromboembolism is a clinical syndrome, a complex of symptoms that occur as a result of a thrombus entering the arteries of the pulmonary circulation. This is an extremely life-threatening disease that develops and proceeds suddenly. There are massive, submassive and recurrent pulmonary embolism, as well as heart attack pneumonia - a consequence of active pulmonary embolism. In the first case, the thrombus is so large that it blocks the pulmonary artery either at its bifurcation site or proximal.
Submassive pulmonary thromboembolism develops as a result of obstruction of the lobar pulmonary artery, and recurrent thrombosis due to frequent embolism of small blood clots that block the lumen of small-diameter arteries. In the case of massive and submassive pulmonary embolism, the clinical picture (hereinafter referred to as the clinic) is bright and develops immediately, and the disease can lead to sudden death. Relapsing pulmonary embolism is characterized by a gradual increase in shortness of breath over several days and the development of cough, sometimes with a coughing up of a small amount of blood.
Patterns of development of pulmonary embolism
For the development of pulmonary embolism, the presence of a source of thrombosis in any part of the venous channel of a large circle of blood circulation or in the right heart is sufficient. Occasionally, thrombi during paradoxical movement through the open oval window of the atrial septum can also get from the left atrium. Then, even with left-sided endocarditis, the development of pulmonary embolism is possible, although such situations are extremely rare and are considered casuistic. And in order to provide unambiguous information that will not cause discrepancies and will not mislead the patient, this publication will not touch on the paradoxical movement of blood clots from the left heart.
As soon as a mobile blood clot forms in the veins of the pulmonary circulation or in the right heart, there is a high probability of it entering the pulmonary artery. The most common source of blood clots are varicose veins of the lower limbs and pelvis. In the area of venous valves, due to stagnation of blood, a parietal thrombus is gradually formed, which is initially attached to the subendothelial lining of the vein. As it grows, a part of the thrombus comes off and goes to the right heart and lungs, where it causes thromboembolism of the pulmonary artery or its branches.
The mechanism of development of pulmonary embolism
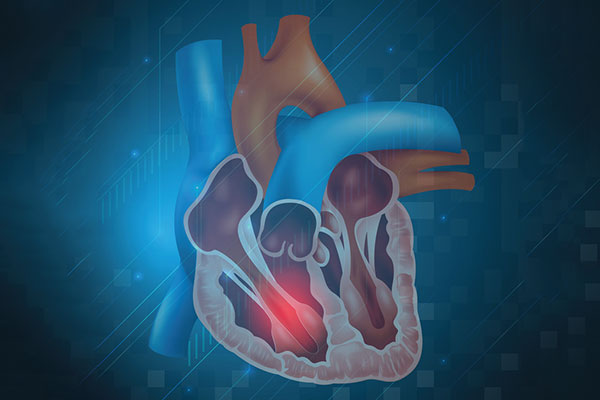
Through the right atrium and right ventricle, a blood clot enters the trunk of the pulmonary artery. Here it irritates the receptors, causing pulmonary-cardiac reflexes: increased heart rate, increased minute volume of blood circulation. That is, the body responds to a signal about irritation of the receptors of the pulmonary artery with increased cardiac activity, which is necessary to push the blood clot into narrower sections of the arterial bed and minimize the consequences of the disaster. This complex of disorders is already called pulmonary embolism, the symptoms and severity of which linearly depend on the size of the thrombus.
In a certain area of the pulmonary pool, despite attempts by the cardiovascular system to push the blood clot further, the latter will certainly get stuck. As a result, systemic arteriospasm instantly develops, blood flow in the affected area of the lung is blocked. With massive pulmonary embolism, it is impossible to push a large thrombus into a small-caliber artery, and therefore total obstruction develops.
As a result, the blood flow to the main sections of the pulmonary circle of blood circulation is blocked, and therefore oxygenated blood does not flow to the left parts of the heart - the collapse of the large circle of blood circulation develops. The patient instantly loses consciousness due to brain hypoxia and shock, arrhythmic activity of the heart is provoked, ventricular extrasystole develops, or ventricular fibrillation starts.
Signs of massive and submassive embolism
The above example demonstrates acute pulmonary thromboembolism, which rarely helps. As a rule, similar clinical situations occur in postoperative or long-term immobilized patients after the first rise. Outwardly, it looks like this: the patient rises to his feet, due to which the venous outflow from the veins of the lower extremities is accelerated and the separation of the thrombus is provoked. In the inferior vena cava, it rises and causes pulmonary thromboembolism.
The patient screams from pain and shock, loses consciousness and falls, ventricular fibrillation develops, breathing stops, and clinical death occurs. As a rule, with pulmonary embolism it is very difficult to stop ventricular fibrillation, since it is associated with myocardial hypoxia. Its elimination in case of massive embolism is almost impossible, which is why it is impossible to help the patient with total obstruction and the development of arrhythmia even with an instant diagnosis and the start of therapy. In addition, the rate of development of arrhythmia is so high that clinical death develops even before people in the same room as the patient manage to call for help.
Subtotal PE
In the case of subtotal pulmonary embolism, the rate of development of symptoms is much lower, but this does not reduce the risk to life. Here, the branch of the lobar pulmonary artery is obstructed, and therefore initially the volume of the lesion is much smaller. The patient does not lose consciousness abruptly, and arrhythmia does not develop suddenly. However, due to the development of reflex reactions of arteriolospasm and the appearance of shock symptoms, the patient's condition worsens sharply, severe shortness of breath develops, and the severity of acute heart and respiratory failure increases.
In the absence of treatment for pulmonary embolism and the impossibility of thrombolysis, the probability of death is about 95-100%. Relatives of the patient should understand that such a patient requires emergency thrombolytic therapy, and therefore it is impossible to hesitate in going to the ambulance. For comparison, with thromboembolism of the branches of the pulmonary artery, where the vessels of small caliber are obstructed, the patient can survive without medical assistance.
It is to survive, because we are not talking about a quick recovery, but about survival with current disorders in the work of the cardiovascular and respiratory systems. The severity of his condition will gradually increase with the worsening of shortness of breath, hemoptysis and the development of heart attack pneumonia. If these symptoms appear, you must immediately contact the emergency room of the hospital or emergency medical care.
Causes of pulmonary embolism
Any phenomenon that provokes the development of vein thrombosis of the lower extremities or the pelvis, as well as the formation of small blood clots in the right atrium or on the right atrioventricular valve, can cause pulmonary embolism. The causes of pulmonary embolism are as follows:
- varicose leg disease with phlebothrombosis, acute thrombophlebitis without taking anticoagulants;
- paroxysmal or permanent atrial fibrillation without anticoagulant therapy;
- infectious endocarditis of the right heart;
- prolonged patient immobilization;
- traumatic surgery;
- long-term course of oral contraceptives;
- oncological disease of the kidneys, metastases along the inferior vena cava and renal veins, hematologic diseases;
- hypercoagulation, thrombophilia, DIC;
- recent fractures of the pelvis or tubular bones of the body;
- pregnancy and childbirth;
- obesity, metabolic syndrome, diabetes mellitus;
- smoking, high blood pressure, sedentary life.
These causes can lead to pulmonary embolism. Diagnosis and treatment of these diseases, as well as taking anticoagulants, can eliminate or significantly reduce the risk of pulmonary embolism. For example, anticoagulants are included in the standards for treating fractures during rehabilitation after their healing, as well as after surgical operations and delivery.
These drugs are also indicated for atrial fibrillation and infectious endocarditis with vegetations on the heart valves. Such conditions often cause thromboembolism of small branches of the pulmonary artery, rather than massive and submassive pulmonary embolism. However, these are still serious diseases requiring medical attention. The most effective drugs for prevention are new oral anticoagulants (PLA). To receive them, INR control is not required. They also have a constant anticoagulant effect, which is independent of nutrition, as in the case of the drug "Warfarin".
Diagnosis at the prehospital stage
Regardless of the qualifications of medical personnel with massive pulmonary thromboembolism, the clinic, diagnosis and treatment can fit in the first 30 minutes, especially in the case of rapid development of arrhythmia and clinical death. Then the patient quickly dies, although the diagnosis itself is not in doubt. Often, pulmonary embolism is detected at the stage of the SMP, and the main diagnostic symptoms are:
- complaints of sharply arisen severe pressing and stitching “dagger” pains in the chest, after which the patient screams and sometimes falls unconscious;
- sharply appeared shortness of breath, severe feeling of lack of air and squeezing in the chest;
- palpitations with the development of pain in the heart, irregular heartbeat;
- the sudden appearance of a dry cough at first against a background of full health, and then with bloody sputum;
- sharply developed cyanosis (bluish-cyanotic color) of the lips, gray (earthy) complexion, swelling of the veins of the neck;
- decrease in blood pressure with massive or sharp increase in blood pressure with submassive and recurrent pulmonary embolism, fainting or loss of consciousness.
The main goal of diagnosis for such symptoms is to exclude myocardial infarction. If the ECG does not have signs of transmural infarction, then with a high degree of probability the current state should be interpreted as pulmonary embolism and provide appropriate emergency care. With pulmonary embolism, an ECG may indicate: inversion of the T wave and the appearance of the Q wave in lead III, the appearance of the S wave in lead I. One of the diagnostic criteria is the expansion of the P wave and the increase in its voltage in the initial segment. Also, changes on the ECG are “volatile”, that is, they can change over a short period of time, which indirectly confirms pulmonary embolism and reduces the number of convincing criteria in favor of myocardial infarction.
With recurrent pulmonary embolism, the symptoms, treatment and diagnosis are somewhat different, which is associated with a much smaller lesion volume. For example, if with a massive pulmonary embolism, the size of the thrombus is about 8-10 mm in width and from 5-6 to 20 cm in length, then with a relapsing lung, many small clots 1-3 mm in size fall into the lung. Because of this, the symptoms are much poorer and include shortness of breath of mild or moderate severity, cough, sometimes with a small amount of blood, and hypertension. These symptoms increase for some time, mimic pneumonia or progressive angina pectoris, especially if they are not accompanied by hemoptysis.
Prehospital treatment
Treatment includes oxygen therapy with 100% oxygen, preferably mechanical ventilation, narcotic analgesia (morphine or fentanyl, neuroleptanalgesia is allowed), anticoagulant therapy with unfractionated heparin 5000-10000 IU, thrombolysis with Streptokinase 250 000ED with preliminary administration of Prednisolone 90 mg.
In addition to this treatment for pulmonary embolism, infusion therapy and compensation for existing disorders are required: defibrillation with appropriate arrhythmias and cardiotonic drugs for hypotension. The indicated treatment is highly effective, but it will not help to completely dissolve the thrombus - hospitalization in the intensive care unit is required.
It is important to understand that the cost of error at the prehospital stage may not be crucial in terms of prognosis for the patient. For example, in the case of changes on the ECG that are characteristic of a heart attack on the background of developing pulmonary embolism, narcotic analgesia and anticoagulant therapy with similar drugs are also indicated. Only the appointment of nitrates can cause harm, which will accelerate the drop in blood pressure.
Patients and SMP staff also need to remember that with myocardial infarction with low blood pressure (less than 100 \ 50 mmHg) or suspected pulmonary embolism, nitrates cannot be taken. Thus, the provision of care to a patient with pulmonary embolism is almost the same as for myocardial infarction with left ventricular failure amid hypotension. This means that the SMP employee has additional time for diagnosis against the background of the started effective treatment of pulmonary embolism.
Diagnosis of pulmonary embolism at the hospital stage
Diagnosis and treatment of pulmonary embolism at the hospital stage is more effective than prehospital. This is partly a purely statistical conclusion, because due to massive thromboembolism, they often do not even end up in hospital because of the high prehospital mortality. And in the case of submassive pulmonary embolism, heart attack pneumonia and recurrent thromboembolism of the pulmonary artery disease “gives time” for high-quality diagnosis and treatment. Identified symptoms are similar to those that occurred during the diagnosis at the prehospital stage.
The exclusion of a heart attack by ECG and the appearance of signs of overload of the right heart immediately directs the doctor towards pulmonary embolism. To confirm the diagnosis, x-rays, emergency laboratory tests are performed: a quantitative analysis for D-dimers, troponin T, KFK-MB, myoglobin. With pulmonary embolism, D-dimers significantly increase with a normal troponin index (a marker of myocardial infarction).
The gold standard for diagnosing pulmonary embolism is the rarely available method of angiopulmonography or perfusion scanning. He is able to reliably confirm or refute the diagnosis of thromboembolism, however, such a study is not possible in most hospitals, or because of the severity of the condition, the patient dies before it. Diagnostic assistance is also provided by echocardiography, ultrasound of the veins of the lower extremities, and dopplerography. Intraoperative catheterization of the right atrium and determination of pressure can be performed, which will confirm pulmonary hypertension.
Hospital therapy
Hospital treatment of pulmonary embolism requires careful monitoring of the patient's condition in the intensive care unit. After confirming the diagnosis, it is necessary to start thrombolytic therapy with tissue plasminogen proactivators - “Tenecteplase” or “Alteplase”. These are new thrombolytic drugs, the main advantage of which is the absence of thrombus fragmentation. They lyse it, as it were, in layers, in contrast to Streptokinase.
Thrombolytic therapy (TLT) is designed to dissolve a blood clot, if possible. – , , .
, « » . . – , .
: , , , . , – , « » - . , .