Lymphoblastic leukemia of the blood is considered the most common oncological pathology of children. It accounts for approximately 25% of the total number of cancers detected in pediatrics. Next, we consider in more detail blood leukemia - what it is, why it appears and what therapeutic measures are carried out with this pathology.
General information
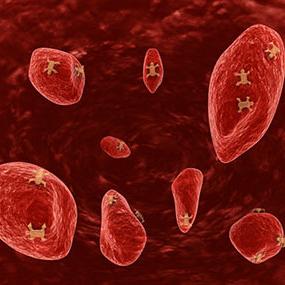
Blood leukemia - what is it? This disease belongs to the group of oncological. ALL (acute lymphoblastic leukemia), the symptoms of which will be discussed below, is a group of heterogeneous neoplasms from cells that have certain immunophenotypic and genetic characteristics. Secondary anomalies of proliferation, differentiation, or both contribute to an increase in the production and accumulation of these elements in the bone marrow. As a result, the cells infiltrate parenchymal organs and lymph nodes. Most (about 80%) of all leukemia (leukemia) detected in children is of a lymphoid nature.
Prevalence
Malignant blood diseases today are found everywhere in the world. The prevalence of ALL in developed countries is 3-4 cases per hundred thousand children annually. In Central Asia and Africa, pathology is less common. Often ALL is noted in the USA, Japan, China, Europe. The peak incidence in children is considered the age of 2.5-5 years. More often, the pathology develops in boys.
Predisposing factors
First of all, they include the age of the mother in the prenatal period, the large weight of the newborn is more than 4000 g, post- and prenatal exposure to ionizing radiation. In what cases can acute lymphoblastic leukemia still occur? The maternal medical history may contain information about fetal death in a previous pregnancy. This could be due to adverse environmental conditions or due to a genetic predisposition. In the case of cancerous relatives in the family, the likelihood that future generations will have acute lymphoblastic leukemia increases. The causes of the disease may be associated with syndromes of instability of chromosomal elements. These include, in particular, Down syndrome, neurofibromatosis, variable immunodeficiency, Fanconi anemia, X-linked agammaglobulinemia (congenital) and others. As a result of a number of studies, experts came to the conclusion that in acute lymphoblastic leukemia, as in the development of other oncologies, spontaneous mutation of progenitor cells occurs. It is subsequently complicated by triggering environmental factors that activate proliferation. These are the most common phenomena that can trigger leukemia. The causes of pathology are one of the fundamental points in choosing therapeutic methods.
Diagnostics
When identifying any pathology of an oncological nature, the clinical characteristics and signs of the cells that make up the tumor substrate are taken into account. The diagnosis of ALL is made on the basis of paraclinical and physical examinations, medical history and laboratory tests.
Clinical picture
Signs of leukemia are a complex of several syndromes:
- Intoxication. In acute lymphoblastic leukemia, malaise, weight loss, weakness, and fever are noted. The latter can be triggered by a viral, bacterial, protozoal (rarely) or fungal infection, especially in patients with neutropenia.
- Hyperplastic. In acute lymphoblastic leukemia, spleen and liver infiltration occurs. This, in turn, leads to hepatosplenomegaly, which can manifest as soreness in the abdomen. The first signs of leukemia are pathological fractures of the tubular bones or spine. Soreness and swelling of the joints can initially be mistaken for manifestations of rheumatoid arthritis or other disorders. Bone damage - for osteomyelitis. With leukemic infiltration of the joint capsule and periosteum, bone infarction and tumor enlargement of the bone marrow in volume, extensive pain appears. Along with this, changes characteristic of the pathological state are revealed on the radiograph. They are especially clearly visible near large joints and in tubular bones. Soreness can occur later, due to aseptic necrosis and osteoporosis.
- Anemic. In acute lymphoblastic leukemia, tachycardia, pallor, bleeding of the mucous membranes in the mouth, hemorrhagic syndrome on the skin are noted. Due to intoxication and anemia, weakness develops.

Manifestation of pathology
In 5-30% of cases of primary acute lymphoblastic leukemia in boys, an initial increase in the testes is observed. Bilateral or unilateral dense, painless infiltrates are noted. In practice, cases of a significant increase in kidneys have been reported. In this case, there may be no clinical manifestations of their lesions. Rare complications include effusion pericarditis and myocardial infiltration against the background of lymphatic obstruction between the epicardium and endocardium. With an increase in lymph nodes in the mediastinum, disturbances in the activity of the respiratory system can occur. These signs of T-cell type leukemia lead to the development of the superior vena cava syndrome . Respiratory failure may also occur. In some cases, leukemic infiltration of the lung tissue or hemorrhage in them is noted. Sometimes it is difficult for specialists to differentiate these complications from infectious pathologies. Among the common signs of eye damage against acute lymphoblastic leukemia, retinal hemorrhage, swelling of the nipple in the optic nerve, and vascular infiltration should be noted. With ophthalmoscopy, plaques at the bottom of the eyeball can be detected. The presence of dense cyanotic infiltrative painless elements on the skin is also likely. With any damage to the cover, an infection can develop. In this regard, in the process of diagnosis, panaritiums, paronychia, infected bites of various insects, traces of injections, etc. can be detected.
Paraclinical studies: KLA
Hemoglobin can be reduced or normal. Hematocrit and red blood cell count are usually reduced. A decrease in the number of reticulocytes is noted. The white blood cell count may be reduced, elevated, or normal. However, in this case, not in all cases imperious cells can be detected. Pathology is characterized by a "leukemic failure." We are talking about the presence of power cells against the background of the absence of intermediate forms - metamyelocytes and myelocytes - in the blood formula. Thrombocytopenia is commonly observed.
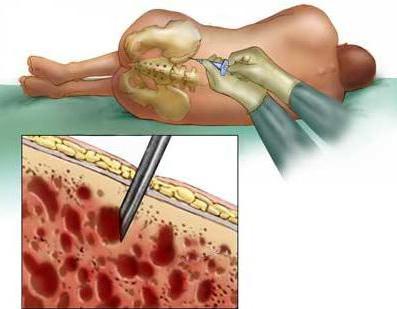
Myelogram
This procedure is a capture of bone marrow puncture. The material must be taken from at least two points. The procedure is preferably performed under general anesthesia. In children older than two years, puncture is taken from the anterior and posterior iliac crests , up to 2 years - from the heel segments or tuberosity of the tibia. In a cytological morphological study, as a rule, hypercellular bone marrow material with narrowed shoots of the normal hematopoiesis system and infiltration by blast cell structures is detected.
Cytochemical study
This is one of the essential stages of diagnosis. Using cytochemical staining, it is revealed which line the cells belong to. Necessarily applied research on myeloperoxidase.
Spinal puncture
This is also a mandatory diagnostic procedure for suspected acute lymphoblastic leukemia, the causes of which are indicated above. Spinal puncture should be performed in conditions of sedation and in the case of the presence in the peripheral blood of at least 30 thousand / μl of platelets. If necessary, thrombus suspension transfusions are performed before the procedure. In order to prepare a cytopreparation, at least two milliliters of cerebrospinal fluid will be required. If power elements and signs of damage are found in the cranial nerves, a diagnosis of neuroleukemia is made - leukemic damage to the central nervous system. However, it should be noted that the penetration of lymphoblasts into the nervous system and infiltration of the meninges occur in all cases, even in the absence of clinical and laboratory manifestations. It is also desirable, and when identifying neurological symptoms, it is necessary to conduct a computer or magnetic nuclear tomography of the spinal cord or brain.

Other studies
With the help of ultrasound of the retroperitoneal space and the abdominal cavity, it is possible to clarify the size of the parenchymal infiltrated organs, enlarged lymph nodes in the abdominal cavity and other areas, organs in the pelvis, and testicles. As part of the diagnosis, chest radiography is performed in two projections. This is necessary to detect an increase in the mediastinum. If indicated, radiography of the joints and bones is prescribed. As part of laboratory research, a biochemical analysis is performed. He, as a rule, shows an increase in LDH of more than 500 IU, probable disturbances in the activity of the liver and kidneys. Before starting chemotherapy, echocardiography and ECG are recommended. Today, among other methods, molecular genetic and cytogenetic methods for determining the number of chromosomes, as well as their structural changes, are used in the study of affected cells.
Therapy: General Information
The basic principle on which modern pediatric oncohematology is based is the division of patients into groups according to the intensity of therapy. It is selected depending on the severity with which acute lymphoblastic leukemia occurs. The prognosis of the condition is also of great importance. So, for example, those who need moderate chemotherapy to eliminate the pathology are categorically not recommended to receive more toxic and severe drugs. At the same time, for those whose estimated survival is not so high, the intensification of measures may be a chance for recovery. When dividing into groups of patients diagnosed with leukemia, the prognosis is made on the basis of previous experience, as well as individual protocols entered into the classification system. In each of them, one or another strategy of therapeutic measures of a certain intensity is formed. Under the existing classification, a general agreement has been adopted on the distribution among patients at risk of the diagnosis of acute lymphoblastic leukemia. Children's treatment was developed back in the late sixties of the last century in America. By and large, the principles on which therapeutic tactics are based have not undergone any particular changes. In patients under the age of one year, the pathology manifests itself in an extremely aggressive form and is characterized by neuroleukemia, leukocytosis.
The main therapeutic methods
The treatment uses drugs such as Prednisone and Vincristine. Endolumbar administration of Methotrexate and cranial irradiation to prevent neuroleukemia are also used. A special treatment program has also been developed. This means that all patients received clearly defined dosages and combinations of chemotherapeutic agents in a specific time frame, according to the protocol. By the end of the seventies, it became clear that after undergoing such a program, about 50% of children who were diagnosed with leukemia recovered. The reasons for further progress in the treatment of pathology are due to the determination of heterogeneity of ALL and the introduction of international cytological classification systems and prognostic factors, the distribution of patients into groups, and the development of differentiated programs. The organization of multicenter studies, the study of the pharmacokinetics of various cytostatic agents for the formation of more effective chemotherapeutic regimens, as well as the intensive development of accompanying events were of great importance.

The basic principles of therapy
Thanks to the activities described above, new generation chemotherapy programs have been created. Most of the protocols used today are based on the principles of initial intensive care, the purpose of which is the maximum destruction of the pool of pathological cells. The creation of therapeutic programs is based on the use of cytostatics in the form of successive combinations (rotation), high-dose chemotherapeutic regimens, as well as the intensive prevention of pathology.
Features of the use of drugs
The main therapeutic and prophylactic measures for neuroleukemia are intrathecal administration of Prednisone, Cytosar, Methotrexate (in dosages according to age) and cranial irradiation. The latter is carried out at the initial stages of therapy. With endolumbar administration, the drug "Methotrexate" has a systemic effect. In this regard, to reduce the tumor mass, it is necessary to conduct the first lumbar medical puncture early. Cranial radiation has distant and immediate side effects. In this regard, studies on the optimization of ALL therapy, conducted today, are aimed at reducing the dose and clearly identifying patients from the low-risk group, for whom this radiation therapy is not mandatory. All these achievements made it possible in the late eighties of the Goths of the last century to overcome the 70 percent barrier to five-year survival in children with leukemia without relapse.
Modern therapeutic programs
The treatment that is used today includes several phases. The first is the induction of remission using three or more agents that are administered over 4-6 weeks. The second is multi-agent consolidation of the previous phase. The third is maintenance therapy. As a rule, antimetabolites are used in the last phase for 2-3 years. Accompanying therapy helps to prevent and eliminate many of the complications associated with induced cytopenia and immunosuppression. The need to use supportive therapy for 2-3 years was proven back in the middle of the last century. Usually during this period, the patient takes the drug "6-Markaptopuriin" every day. Weekly, he is given Methotrexate. Depending on the number of leukocytes, the dosage is established. As practice shows, patients have a satisfactory tolerance of such a therapeutic regimen. The implementation of supportive measures at 80% of the required volume is considered an unfavorable prognostic factor in terms of relapse.
additional information
There are a number of problems in the treatment of ALL. In particular, the number of patients with mutant clones of tumor cells resistant to chemotherapy is increasing, the high cost and the appearance of late side effects (neuroendocrine disorders, growth disorders, secondary tumors). Failures of induction treatment are due to the early death of patients due to toxic complications or a resistant tumor. Also, approaches to the treatment of patients who did not respond to the standard regimen are very limited. As an alternative, such agents as Teniposide, Vepesid, and Cytosar are used. Today, about 70% of children have a 5-year remission. Acute lymphoblastic leukemia in adults recurs in every seventh case. This suggests that the duration of the period of remission can be achieved only in 20% of cases. As a rule, the return of pathology is noted in the first 2 years after diagnosis. The state of remission is characterized as the absence of power cells in the blood, the presence of less than 5% of blasts in the bone marrow tissue, the appearance of signs of restoration of hematopoiesis. When analyzing cerebrospinal fluid, less than 5 mononuclear cells / microliter are detected. For the success of treatment, it is necessary to quickly achieve a state of remission. In 90% of patients, as a rule, abnormal cells are sensitive to chemotherapy.
Finally
The main goal of therapy is to rid the patient of the pathology and return him to a normal social life and to a good state of health with a minimum of complications due to treatment. To achieve this today is quite difficult. This is due to the fact that most anti-leukemic medicines are not sufficiently selective and toxic. However, advances in understanding the clinical and biological heterogeneity of pathology, the constant conduct of various studies give hope that the molecular pathogenesis of the disease will still be deciphered to the end. In this case, knowledge of the mechanisms of tumor transformation will allow the development of more effective and least toxic therapeutic agents.