In the ICD, the vertebral hemangioma is encoded with the D18 code, and is included in the subgroup of benign formations D10-D36. Currently, doctors say, among all vascular tumors, this is the most common. About 10% of the world's population suffer from the presence of hemangiomas of different localization regions. The predominant share among them is women. The average age of patients is estimated at 20-30 years. For women over 40, the probability of hemangioma is about 80%.
general information
Often, the hemangioma of the vertebral column body for many years does not manifest itself with any symptoms, and the only way to identify it is to undergo a full preventive examination. If the disease is still accompanied by symptoms, the first manifestation becomes soreness, which stimulates you to see a doctor.
In order to identify the causes of the syndrome, an x-ray, MRI is prescribed. During such events, hemangioma is not difficult to determine. As the diagnosis is made, the doctor determines how reasonable it is to operate on the patient. As is known from medical statistics, hemangioma is not prone to degeneration, but can cause complications, therefore serious and responsible treatment is required.
Relevance of the issue
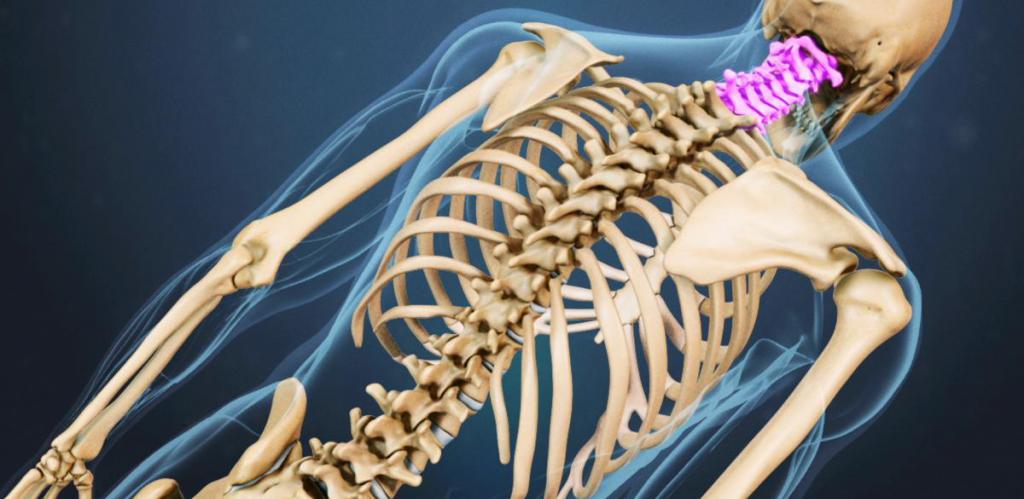
It is impossible to overestimate the importance of the spine for human life. The spinal column is the support of our body, which keeps the spinal cord safe. Only thanks to the functionality of the spine can a person feel temperature changes, feel pain and touch, move, controlling the activity of all parts of the body. Internal organs are completely subordinate to those signals that are sent to them from the spinal cord.
Often the hemangioma of the thoracic vertebrae (and other departments) is localized strictly inside the vertebra, therefore it does not affect the brain located nearby. If the vertebral structures are broken for any reason, integrity suffers, if the vertebral column becomes fragile and unstable, displacements, fractures, and compression of vital elements are possible. From statistics it is known that more often several vertebrae suffer at once. The most typical combination is chest and lumbar at the same time.
The nuances of the disease
What is hemangioma of the vertebra L1 (and any other)? The term is used to denote such a vascular neoplasm that visually looks like a ball of interwoven various vessels. These areas under the influence of pathological processes undergo changes. As a rule, with hemangioma, the vertebral body is harmed. Sometimes the tumor grows in the layers of cartilage between the vertebrae.
The start of hemangioma growth is the formation of inferior vessels. It is from them that a tumor gradually forms. Excessive stress or trauma causes hemorrhage, a blood clot appears, and blood activates osteoclasts. Cells are trying to remove organic structures from the affected area that should not be here. The space that is freed up at the same time is almost immediately filled with inferior vessels. The process is continuous, with time the hemangioma increases in size. As a rule, the size is no more than 1 cm, although in rare cases larger formations are possible.
Risk group
It is known that hemangiomas are more likely to occur in women than in men. The risk group includes people who have experienced an injury to the spinal column.
Statistical studies have shown: if among close relatives there are people who have undergone vascular neoplasms in the spinal column, the probability of hemangioma is five times higher compared to those who do not have such closest relatives. Doctors suggest that the phenomenon can be explained by inherited insolvency of the vessel walls, which leads to a transformation, against which sooner or later treatment of vertebral hemangioma is required.
Since the neoplasm is much more common in women than in men, scientists have concluded that the presence of estrogen in the circulatory system affects its appearance. It was also revealed that the formation is particularly active in the third part of the gestation period. There are two immediately affecting factors - a displaced hormonal balance and an increased load on the musculoskeletal system.
Important Nuances
Hemangioma of the vertebra may appear as a result of excessive load on the spinal column. A similar cause is the injury sustained by this organ. The vascular component, under the influence of aggressive influence, can begin expansive growth, which leads to neoplasm. If a hemangioma is already present, a mechanical external influence activates the growth of the formation.
Statistics show that hemangioma of the thoracic vertebra is common. In medicine, this area is encoded by the letters Th12. The second most frequently affected area is the lower back. Among the most dangerous is a neoplasm in the neck. With such a hemangioma, there is a possibility of a disruption in the supply of blood to the brain. In the lumbar region, the hemangioma is most often localized near the elements L1-L4. Possible complications associated with such a tumor are neurological disorders.
What happens?
There are two main types of vertebral hemangioma: aggressive and non-vertebral. The aggressive form is diagnosed if the neoplasm grows rapidly, leads to compression syndrome, and provokes pain and a vertebral fracture. On average, aggressive hemangiomas occur in 10% of all patients with this diagnosis.
Non-aggressive vertebral hemangioma is characterized by a favorable course. Formation is gradually developing, but processes are slow, rarely manifest themselves in symptoms. If the tumor is small, it may disappear on its own over time.
To assess the case and formulate forecasts, it is necessary to analyze the size of the hemangioma. Sometimes the area of damage is the vertebral body, possibly spreading to a half ring in the back. There are situations when the hemangioma affected the vertebra completely. There is a risk of epidural development when the area above the soft membrane of the brain is covered.
Specificity check
If hemangioma of the C6 vertebra or any other is established, it is necessary to take tissue samples from this area for histological analysis. Based on the characteristics of the tissues, the case is considered cavernous, capillary or mixed. Cavernous is called such a hemangioma, when the neoplasm consists of blood-filled vascular cavities. This form of the disease is characterized by a fairly strong pain syndrome. The probability of a vertebral fracture is relatively high.
Capillary hemangioma is formed by small capillaries. Mixed has features of both types.
Features of the case will depend on the structure of the neoplasm, its dimensions and the area of localization. It also determines symptoms and prognosis. Only after evaluating all the specific aspects, the doctor will determine which approach to treatment is most effective.
How to notice?
Symptoms of a hemangioma of the vertebra are determined by the location, size of the neoplasm, and features of the location relative to the vertebral body. As a rule, a neoplasm develops for a long time, without manifesting itself in any way, without disturbing the patient. At this stage, hemangioma can only be detected by chance, if you go to the doctor because of an injury or because of other impaired functionality, the health of the spinal column. A full examination of the area allows you to notice a vascular tumor.
As a rule, the first sign of vertebral hemangioma, noticeable to a person, is the pain of a separate area. At first the pain is intense, comes in bouts. Over time, the hemangioma increases in size, along with this, the pain also becomes larger, gradually becoming intolerant.
Nuances and diagnosis
Neoplasms are considered dangerous, the size of which is more than a centimeter. These can not only stimulate very severe pain, but can also cause neurological disorders due to compression of the structures of the spinal cord and a violation of the tissues that form the vertebra.
If the hemangioma is relatively small, it provokes a moderate level of pain, the symptoms become stronger during a night's rest or after physical activity. Pain is disturbed only by that part of the spine where the neoplasm is localized.
If the hemangioma of the vertebra spreads to the spinal cord, damages its structures, additional phenomena are possible that indicate a disease. The patient suffers from paralysis, paresis, numbness of certain parts of the body is possible. Sometimes the functionality of the pelvic organs is impaired.
Localization - Neck
Hemangioma of the cervical vertebra manifests itself as soreness of this part of the body and numbness of the arms and legs. Occasionally, paralysis, paresis. The patient complains of a violation of the rhythm of the heartbeat. Sometimes, against the background of hemangiomas, the digestive system or pelvic organs go astray.
Violation of the structure and functionality of the cervical spine can adversely affect the quality of blood supply to the brain structures. This leads to headaches and impaired human cognitive abilities. Sometimes dizzy, vision suffers, hearing deteriorates.
Lumbar tumor
Among all the possible options, the treatment of hemangiomas of the vertebral body L3, L1, L2, L4 is required very often - only localization in the thoracic region is more common. It is possible to suspect the presence of hemangioma in the vertebral part if the legs are numb, paresis and paralysis are localized here. The tumor can manifest itself as pain, covering the lower back, spreading to the groin, thigh. Violations of the functionality of the pelvic organs are especially pronounced if the third and fourth vertebrae of the department are affected.
Aggressive hemangioma can cause sexual impotence, the impossibility of conception.
Timeliness and care are the key to health
Aggressive swelling can lead to serious consequences. Vertebral fractures due to pressure, compression of the brain, brain roots are possible. In this case, paralysis, paresis become persistent, it is not possible to reverse the negative processes in internal organs and systems. To prevent such an outcome, it is important to use the help of a doctor at the first doubtful symptoms.
If it is possible to detect hemangioma early, choose the appropriate method of treatment, complications can be avoided and irreversible harm to the brain can be prevented. To make a diagnosis, you will have to undergo examination by a surgeon, neurologist, vertebrologist.
Diagnostics
If hemangioma of the lumbar vertebrae, thoracic, cervical vertebrae is assumed, it is necessary to first refer the patient to an x-ray. The procedure is done from different angles. The method is simple, cheap to implement, available in almost any clinic.
To clarify the case can be sent to CT, MRI. The second method is especially effective and informative, gives an idea of the harm received by the vertebra, allows you to assess the condition of the soft tissues of the affected area nearby.
What to do?
The treatment of hemangiomas of the vertebral body is selected based on the characteristics of a particular case. It must be understood that the process is not easy in any case - localization imposes significant restrictions on the possibility of medical manipulations. If you simply remove tissue from the body, the vertebra will become unstable. This can trigger a fracture. During such careless treatment, the spinal cord is likely to suffer. Perhaps a violation of the integrity and functionality of the brain roots.
To find a rational way to get rid, you need to visit a neurosurgeon. The doctor will determine the size of the hemangioma of the vertebral body, other parameters of the neoplasm, on the basis of which he will propose the optimal strategy.
Surgery or not?
If the neoplasm is small, does not manifest itself with symptoms, the patient is registered, they are offered regular MRI scans to monitor development, but they do not take any active steps.
Surgical intervention is recommended if the size of the hemangioma of the vertebra is such that its third is covered by a neoplasm or an even larger area is affected. If the tumor develops rapidly and grows, is aggressive, leads to complications, compression of the brain or roots is observed, a fracture, and removal is also indicated.
Spinal column surgery is possible only in a specialized center with a neurosurgeon and the equipment necessary for his work. Qualification of a specialist, his experience in many respects affect the result.
Conservative treatment for this course of the disease can alleviate the symptoms, but it is impossible to achieve a complete cure. Drugs are prescribed for the relief of pain, inhibition of foci of inflammation.
What are the options?
In some cases, the patient is offered a resection of the vertebra. This approach is classic, it allows you to remove a diseased area from the body.
A possible option is vertebroplasty, performed by punctures through the skin. In recent years, the use of laser has gained popularity. Known approaches - alcoholization of the tumor, vascular embolization.
For the first time, a successful operation according to the classical technique was carried out in the first third of the last century. Currently, this approach is considered far from the most optimal, since there is a high probability of complications. Often the vascular region becomes a source of bleeding, and during the intervention, the systems responsible for brain nutrition can be disrupted. There is a risk of a vertebral fracture.
Method conditions and features
Classical surgery is used only in the absence of alternative options and only in a situation where hemangioma is accompanied by compression of the brain, brain roots. With an open operation, there is no way to completely remove the neoplasm - these are the features of the technique. The doctor using special equipment removes epidurally located elements.
If classical intervention is the only option possible in a particular case, resort to a decompression approach. As part of the operation, the doctor eliminates the pressure from the education on the spinal cord.
From medical statistics it is known that children often need such an operation. This is explained by the impossibility of using a cementing substance, since it will block the ability of the vertebra to grow, which means it will cause serious deformations in the future.
Options and approaches: what are the nuances?
Alcoholization with hemangioma involves the injection of ethyl alcohol into the neoplasm. There is a narrowing of the vessels, as a result of which the dimensions are reduced. This method shows good results, but there are also disadvantages. Bone tissue weakens, leading to destabilization of the area. A few months after alcoholization, the likelihood of a pathological fracture increases. Due to this feature, the treatment method for hemangiomas is not widespread.
Embolization is a method of eliminating hemangiomas, in which a substance is introduced into the affected area that stimulates vascular embolism and inhibits the nutrition of the site. You can inject drugs into the tumor or areas nearby. The main weak point is the likelihood of relapse, as small vessels remain, which means that the hemangioma continues to receive nutrition. There is also the possibility of harm to the structure of the spine. In some cases of tumor localization, embolization is technically extremely difficult, and there are known cases when it is impossible to perform it in principle. A possible negative consequence of the procedure is an acute failure of blood flow in the channels of the spinal cord.
Radiation treatment
This method is a classic treatment for hemangiomas. The approach is relatively safe, especially compared to open surgery. Weakness - high probability of complications. Against the background of radiation therapy, there is a risk of myelopathy, radiculitis. Some patients suffer from negative skin reactions, while others impair the functionality of the fibers that form the nervous system.
To eliminate the neoplasm, it is necessary to use radiation in a high dose. This method is not acceptable for the treatment of children bearing the fetus of women. During the intervention, the integrity of the vertebra is violated, which can provoke a fracture. Radiation treatment of hemangiomas is usually recommended for elderly patients, for the treatment of which the use of other methods is not recommended because of the increased risks.
The most effective!
The best treatment for hemangiomas available to modern humans is vertebroplasty. Into a vertebra enter: specific substance, titanium, barium sulfate. This allows you to reduce the size of the neoplasm, prevent further growth, stabilize the affected area and reduce the likelihood of a fracture. The puncture approach is currently the recommended way to treat hemangiomas, especially relevant in the aggressive form.