Arthrosis of the knee joint (ICD-10 - M17) is a chronic progressive disease characterized by the development of degenerative-dystrophic changes in the cartilage, subchondral bone, capsule, synovial membrane, and muscles. Manifested by pain and difficulty in movement. The progression of the disease leads to disability. Osteoarthrosis of the knee joints affects 8-20% of people. The frequency increases with age.
Classification Kosinskaya N.S.
There are several classifications - for reasons, for radiological signs. It is more convenient in practice to use the Kosinskaya N.S. classification
- Stage 1 - an x-ray picture of a slight narrowing of the joint space and minor subchondral osteosclerosis. Patients complain of pain in the knee joints during long walks, when climbing or descending stairs. There are no functional disorders of the joint.
- Stage 2 - the joint gap narrows by 50% or 2/3. Subchondral osteosclerosis expressed. Osteophytes (bone growths) appear. The pain is moderate, there is lameness, the muscles of the thigh and lower leg are hypotrophic.
- Stage 3 - the joint space is completely absent, there is a pronounced deformation and sclerosis of the articular surfaces with necrosis of the subchondral bone and local osteoporosis. The patient has no movement in the joint, severe pain. There is muscle atrophy, lameness, deformation of the lower limb (hallux valus or varus).
International Classification of Diseases ICD-10
Deforming arthrosis of the knee in ICD-10 is designated M17 (gonarthrosis). It belongs to the 13th class - diseases of the musculoskeletal system and connective tissue (M00 - M99). Osteoarthritis of the knee joint (ICD-10 code) is in the group - arthrosis M15 - M19.
- If damage to both joints begins without any external cause, then this is the primary bilateral arthrosis of the knee joint. In the ICD-10 - M17.0. It is also called idiopathic arthrosis.
- The next option is another primary arthrosis of the knee joint. In ICD-10 - M17.1. These include unilateral arthrosis. For example, M17.1 - arthrosis of the right knee joint in ICD-10. Arthrosis of the left knee has the same code.
- A common cause of the disease, especially in young people and athletes, is trauma. If both joints are affected, then in the classification it sounds like post-traumatic bilateral deforming arthrosis of the knee joints, the code according to ICD-10 is M17.2.
- In the event of a one-sided defeat, the code changes. According to ICD-10, post-traumatic arthrosis of the knee joint is unilaterally designated M17.3.
- If the patient has a history of causes that led to damage to the structure of the joints, for example, acute or chronic overload, arthritis, arthropathy of various etiologies, somatic diseases with joint damage, then this is secondary bilateral arthrosis. Arthritis of the knee in the ICD-10 occupies different positions depending on the cause.
- M17.5 - another secondary arthrosis of the knee joint, according to ICD-10 - M17.5. This is a unilateral organ lesion.
- Unspecified arthrosis of the knee in ICD-10 - M17.9.
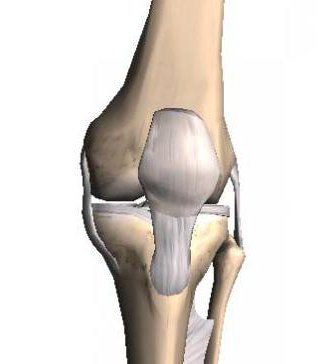
The structure of the knee
The knee joint combines three bones: the femoral, tibial and patella, covering the front of the joint. The connecting areas of the femur and tibia are uneven, so there is a dense hyaline cartilage between them to absorb the load (meniscus). The bony surfaces inside the joint are also covered with cartilage. All components of the joint hold the ligaments: lateral medial and lateral, cruciform anterior and posterior. Outside, it is all covered with a very strong joint capsule. The inner surface of the capsule is lined with a synovial membrane, which is densely supplied with blood and forms a synovial fluid. It feeds all joint structures by diffusion, as there are no blood vessels in the cartilage. It consists of chondrocytes (up to 10%), and intercellular substance (matrix), which consists of collagen fibers, proteoglycans (they are formed by chondrocytes) and water (up to 80%). Proteoglycans, represented by glycosamine glycans and chondroitin sulfate, bind water and fibers .
Etiopathogenesis
The causes of cartilage tissue destruction can be a history of infectious or crystalline arthritis (rheumatoid, reactive arthritis, gout, psoriatic arthropathy), acute or chronic joint overload (sports, weight), trauma, and inactivity in age-related patients. All this causes a metabolic disturbance, a decrease in the level of proteoglycans, and loss of water. The cartilage is pulled, drained, cracked, and thinned. Its destruction occurs, then regeneration with loss of congruency, the bone tissue begins to become bare and grow. If untreated, the joint gap disappears, the bones are in contact. This causes acute pain and inflammation, deformation, bone necrosis.
Clinic
The first manifestations of the disease are pain in the knee joints during physical exertion, after a long walk, when cooled, in cold, wet weather, when climbing and descending stairs, lifting weights. The patient takes care of his leg. Lameness occurs. As the disease develops, crunch, crepitus, difficulty in movement, and joint deformation are noted. Synovitis periodically occurs. On examination, the joint area may be swollen, hyperemic, painful on palpation. Possible deformation of the joint or entire limb.
Diagnostics
To search for the cause of the disease and determine its severity, it is necessary to assign:
- General blood analysis.
- General urine analysis.
- Biochemical analysis: CRP, RF, activity of liver enzymes (AST, ALT), total protein, creatinine, uric acid, glucose.
- X-ray of the knee.
- Ultrasound (if there is a Becker cyst, effusion in the joint).
- During hospitalization, in addition to the studies above, MRI and densitometry according to indications are also performed.
X-ray of the knee joint is done in lateral and direct projections. The radiological signs of arthrosis include: a decrease in the height of the joint space, bone growths, osteophytes, subchondral osteosclerosis, cysts in the pineal glands, deformation.
In the initial stages of the development of the disease, when there are still no radiological signs, magnetic resonance imaging (MRI) will be a more informative method of investigation. This method allows you to see changes in the cartilage, its thinning, cracking, assess the condition of the synovial membrane. Of invasive methods, arthroscopy is informative. It allows you to visually inspect all the internal components of the joint.
Differential diagnosis
Differential diagnosis is carried out in the initial stages of arthrosis, when the clinical and radiological picture is not yet expressed. It is necessary to exclude arthritis of various etiologies: rheumatoid, psoriatic, infectious, reactive, as well as gout, joint damage in ulcerative colitis (ULC), Crohn's disease. With arthritis there will be general and local symptoms of inflammation, corresponding changes in the picture of blood and x-rays. It is necessary to appoint a consultation of a rheumatologist.
Non-drug treatment
Treatment of patients with gonarthrosis is surgical and non-surgical, and it depends on the stage of the disease. At the first and second stages, treatment without surgery is possible. In the second, if there was no effect of conservative therapy, as well as the third, surgical treatment is indicated.
Non-surgical treatment is non-drug and drug. Non-drug therapy includes:
- Weight loss.
- Exercise therapy for strengthening the muscles of the lower leg and thigh.
- Elimination of factors that increase the axial load on the joint (running, jumping, long walking, weight lifting).
- Use of a cane on the side opposite from a sore joint.
- Wearing orthoses to relieve the joint.
- Massage of the muscles of the lower leg and thigh, hydromassage.
- Applied physiotherapy: SMT, electrophoresis with dimexide, analginum, novocaine, ultrasound or phonophoresis with hydrocortisone, chondroxide gel, magnetotherapy, laser. Also, with positive dynamics, paraffin-ozocerite, mud applications are prescribed. Radon, hydrogen sulfide, bischofite baths, hydrorehabilitation have a good effect.
Drug treatment
In accordance with the European Recommendations (ESCEO) 2014 for the treatment of patients with osteoarthritis, an algorithm for the treatment of osteoarthrosis in 4 steps is recommended:
- The first step shows the use of paracetamol on demand for a quick analgesic effect. If the patient has gastrointestinal diseases, it is recommended to combine NSAIDs with gastroprotectors. The reception of structurally-modifying drugs of slow action is shown. These include glucosamine sulfate and chondroitin sulfate. Outwardly on a joint - NSAID ointments. Non-drug therapy methods are also indicated. Each next step does not cancel the previous one.
- At the second stage, patients with severe clinical symptoms (acute pain) or frequent synovitis are prescribed NSAIDs (selective or non-selective, depending on the associated pathology). In case of inefficiency - intra-articular administration of glucocorticoids (with effusion in the joint, the effect is fast, lasting up to three weeks, betamethasone 1-2 ml or methylprednisolone acetate 20-60 mg is injected) or hyaluronic acid (with contraindications to NSAIDs, the pain relief is the same, effect 6 months, up to 2 ml is introduced 3-5 times once a week).
- The third step is the last attempts of drug therapy before preparing for surgery. Weak opioids and antidepressants are prescribed here.
- The fourth step is surgical treatment. Partial or total arthroplasty, corrective osteotomy, arthroscopy are indicated.
Surgery
With arthroscopy, the following are possible: visual inspection inside the joint, removal of cartilage fragments, inflammatory elements, resection of damaged areas, leveling of the cartilage that has become dilapidated, removal of osteophytes. But the main goal of arthroscopy is to make a diagnosis in order to plan further actions.
Corrective osteotomy of the femur or tibia is performed to restore the axis of the lower limb in order to remove the load from the affected area. Indication for this operation is stage 1-2 gonarthrosis with valgus or varus deformity of the lower limb.
Endoprosthetics can be total or partial. It is usually given to patients older than 50 years. Indications are:
- arthrosis of the second or third stage;
- damage to areas of the joint with valgus or varus deformities of the lower extremities;
- bone necrosis;
- contracture.
Resection arthroplasty is performed after endoprosthetics if there is a recurrence of a surgical infection. After this operation, you must walk in an orthosis or with support.
At the terminal stage of arthrosis, when the joint is unstable (hangs), with severe deformation, acute symptoms, when it is impossible to perform arthroplasty due to high risks or not accepting an endoprosthesis, an arthrodesis surgery is performed. This method allows you to get rid of pain and save the limb as a support. Shortening the limb in the future causes the progression of degenerative-dystrophic processes in the spine.