Hepatic encephalopathy is one of the likely complications of liver diseases such as cirrhosis, viral hepatitis, acute or chronic failure. This pathological condition is a damage to the brain and nervous system by ammonia and other toxic products of the intestine. In most cases, patients have a decrease in intelligence, there are mental disorders, disturbances in the emotional and hormonal levels, as well as neurological symptoms. Hepatic encephalopathy cannot be cured, the prognosis for patients is rather pessimistic: in eight out of ten cases, patients fall into a coma, which inevitably leads to death.
Why does the disease develop?
Hepatic encephalopathy belongs to the group of inflammatory diseases that occur against the background of a weakening of the filtering functions of the liver. The causes and mechanism of development of this pathology are not fully understood, which explains the high percentage of mortality among patients. Considering etiological factors, several of its forms are classified:
- Type A: develops against the background of acute liver failure.
- Type B: occurs with cirrhosis.
- Type C: caused by intestinal neurotoxins entering the bloodstream.
The causes of hepatic failure causing type A encephalopathy include the effects of hepatitis, prolonged alcohol dependence and liver cancer. Also, the disease can occur against the background of poisoning with drugs, drugs and chemicals. More rare factors that can provoke type A pathology are:
- Budd-Chiari syndrome;
- consequences of surgery;
- fatty degeneration in pregnant women;
- Westphal-Wilson-Konovalov syndrome.
The second type of hepatic encephalopathy is cirrhosis of the organ, which is characterized by the death of hepatocytes with subsequent replacement of fibrous tissue. The result of such changes are organ dysfunctions. The pathological process can develop against the background of:
- frequent bleeding within the gastrointestinal tract;
- chronic constipation;
- long-term medication;
- infection by infection;
- the presence of parasites in the body;
- renal failure;
- burns, injuries.
The triggers for the occurrence of type C hepatic encephalopathy are not background liver pathologies, but intestinal pathogens and neurotoxins. With this form of the disease, pronounced neurological symptoms are observed. The main cause of hepatic encephalopathy of this type is the rapid growth and division of the intestinal microbiota, which is explained by:
- excessive consumption of protein foods of animal origin;
- consequences of portosystemic shunting;
- the active course of chronic duodenitis, colitis, gastroduodenitis.
Pathogenesis of the disease
To understand what hepatic encephalopathy is in people, one should turn to the physiological characteristics of the human body. As you know, ammonia is produced in our muscles, kidneys, liver and large intestine. In a healthy person, this substance, together with the blood stream, is transported to the liver, where it is converted into urea. This metabolic process prevents the absorption of toxic elements into the bloodstream. With hepatic encephalopathy, metabolism is disrupted and ammonia, entering the bloodstream, affects the central nervous system.
Intoxication is carried out due to the destruction of the blood-brain barrier. Poisoning substances stimulate the production of glutamine, inhibit the rate of oxidation of sugars. As a result, edema is formed, energy starvation of brain cells occurs. In addition, in addition to ammonia, amino acids enter the brain tissue that are concentrated in its structures, causing inhibition of the enzyme system and inhibition of central nervous system functions. As the disease progresses, the ratio of amino acids in the blood and cerebrospinal fluid decreases significantly. Normally, this indicator is within 3.5 units, and with hepatic encephalopathy it barely reaches 1.5.
In a toxic attack, the concentration of chlorine also increases, and the conductivity of nerve impulses slows down. All this leads to acute liver failure and a change in the acid-base composition of the blood (increased amounts of ammonia, fatty acids, carbohydrates, cholesterol), an imbalance of electrolytes. These violations catastrophically affect the state of astrocyte cells, which are the main protective barrier between the brain and the bloodstream, which neutralizes toxins. As a result, there is a significant increase in cerebrospinal fluid volume, which leads to an increase in intracranial pressure and swelling of the brain tissue.
It is noteworthy that a disease such as hepatic encephalopathy can be chronic or occur sporadically, leading to a spontaneous outcome. Often, a chronic form of pathology lasts several years in patients with cirrhosis.
Initial stages and their symptoms
At the beginning of the development of the disease, no obvious symptoms are observed. The first degree of subcompensation can be accompanied by periodic psycho-emotional disorders, mild tremor of the extremities, sleep disturbances, barely noticeable yellowness of the skin and mucous membranes. Patients often notice that they become distracted, inattentive, lose their ability to concentrate on something, but do not attach much importance to these symptoms. Many do not even suspect about hepatic encephalopathy of the first degree, believing that fatigue, recent illnesses, vitamin deficiencies, and other factors serve as the cause of intellectual disorders.
The next stage of encephalopathy has a greater clinical severity. Hepatic decompensation of the second degree is manifested by asterixis (inability to maintain a certain position, tremor of the extremities) and symptoms such as:
- violations of the regime of the day, characterized by stable sleepiness during the day and insomnia at night;
- long-term fixation of the gaze at one point;
- monotonous, slurred speech;
- visual hallucinations;
- forgetfulness;
- gradual loss of writing skills;
- pain in the right hypochondrium;
- increased irritability;
- sudden mood swings: a state of euphoria can suddenly be replaced by apathy.
At the second stage of hepatic encephalopathy, the patient becomes lethargic, withdrawn, slurredly speaks and gives laconic answers to any questions, which are close to yes or no. Against the background of the disease, motor coordination suffers, disorientation in space develops.
Another specific manifestation of this disease are sweeping uncontrolled twitching, muscle tic. Unconscious motor activity occurs with strong muscle tension in the body and limbs. To check if the patient has such a symptom, he is asked to extend his arms in front of him: the test is considered positive if flexion-extensor reflex movements occur in the joints of the fingers, hands. With the course of pathology, the patient ceases to recognize the shape of objects, he develops incontinence of urine and feces.
Irreversible changes in the last stages
Grade 3 hepatic encephalopathy is considered incurable. There are practically no chances for a successful outcome in such patients. This stage in the development of pathology is characterized by stupor - this condition is characterized by deep depression of consciousness with the loss of voluntary activity, but the presence of conditioned and some acquired reflexes.
With the third degree of hepatic encephalopathy, the following clinical manifestations are observed:
- hyperventilation of the lungs (the patient is breathing heavily);
- lethargy, numbness;
- a sweet smell comes from the oral cavity;
- against the background of increased muscle tone, convulsive, epileptic seizures often occur.
A patient suffering from this pathology often freezes in one pose, falls into a stupor. A person can be taken out of a stupor only by physical action, after which weak facial expressions appear in response to pain. In the future, stupor can lead to coma.
The last stage of progressive hepatic encephalopathy is the coma of the patient. A person loses consciousness and reflexes without reacting to stimuli. In isolated cases, muscle clonus is possible, which is characterized by an unconscious manifestation of primitive reflexes (sucking, grasping). The patient's pupils do not respond to light, sphincters are paralyzed, convulsions and respiratory arrest occur. The immediate cause of death in hepatic encephalopathy is brain hydrocephalus, pulmonary edema, toxic shock.
Disease classification
Depending on the severity of the symptoms of hepatic encephalopathy, the disease can occur openly and latently. The hidden nature of the pathology is most dangerous for the patient. By the way, according to statistics, asymptomatic liver encephalopathy is diagnosed in 60% of cases of cirrhosis.
There are also acute hepatic encephalopathy and chronic. The first progresses rapidly, can develop a couple of days before the coma. Signs of chronic hepatic encephalopathy are less pronounced, the course of the disease can be long-term.
Coma on the background of encephalopathy is true (endogenous) or false. In the first case, we are talking about fulminant damage to the central nervous system in people suffering from liver failure or cirrhosis. With hepatic encephalopathy with a chronic course, false (exogenous) coma often occurs. This condition is less dangerous for the patient, and with timely intensive care, doctors manage to bring the patient into consciousness. But, despite this, the forecast leaves no hope: in 90% of cases, patients die within the first month.
Survey
To establish a diagnosis, a neurologist should examine the patient, check his reflexes, conduct a survey, listen to complaints, evaluate the adequacy of responses and behavior. Often, patients are sent to see a doctor along with relatives, who could supplement the description of the course of the disease, help the doctor draw up an anamnesis of past illnesses, patient addictions, bad medication, heredity, etc.
Laboratory and instrumental diagnosis of hepatic encephalopathy is a complex of complex research procedures:
- Biochemical blood test for liver tests. The study allows you to assess the degree of activity of aminotransferases, to determine the level of gamma-aminobutyric acid, bilirubin, ammonia. With encephalopathy in the blood, a decrease in hemoglobin, albumin, prothrombin, cholinesterase is observed.
- CSF analysis. In the composition of the cerebrospinal fluid, an increased presence of protein is detected.
- Ultrasound of the liver, gall bladder and abdominal organs. The study is conducted to determine the causes of liver failure. If the screening is uninformative, liver puncture is performed.
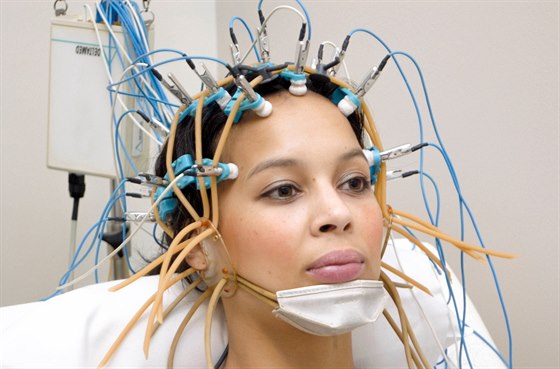
- Electroencephalogram of the brain. The procedure will provide a real idea of the functionality of the central nervous system.
- MRI scan These research methods give a detailed answer about the localization of the affected areas, intracranial pressure, the severity of the patient.
In addition to the basic diagnosis, with liver encephalopathy it is important to conduct a differential study to exclude stroke, rupture of aneurysm, meningitis, alcohol withdrawal.
Treatment of acute hepatic encephalopathy
You need to start the fight against the disease as early as possible. The treatment of the disease is built up with three main stages:
- search and elimination of the factor provoking liver failure;
- a decrease in blood levels of ammonia, chlorine and other toxic substances;
- stabilization of the ratio of brain neurotransmitters.
In acute hepatic encephalopathy syndrome, therapy begins with the use of diuretics. To remove the swelling of the body and internal organs, the brain, "Furosemide", "Lasix" are administered parenterally.
If the patient's mental disorders are too pronounced, sedatives are prescribed. Tinctures of valerian and motherwort may not give the expected effect, as an alternative, they recommend stronger drugs (Haloperidol, Eteperazin, Invega, Rispolept).
If the cause of liver failure was a bacterial infection, antibiotics are prescribed to relieve inflammation. For the treatment of encephalopathy, as a rule, antibacterial agents of a wide spectrum of action are prescribed, which are active in the lumen of the colon in relation to various microorganisms:
- "Neomycin."
- "Vancomycin."
- "Metronidazole".
- "Rifaximin."
In parallel with antibiotics, detoxification solutions are administered intravenously. As soon as the condition stabilizes, they are replaced by nutrient solutions of glucose, sodium bicarbonate, potassium in order to compensate for the deficiency of important trace elements in the body.
With type C hepatic encephalopathy, high cleansing enemas with lactulose are used. To cleanse the intestines, due to which the formation of ammonia is reduced, its absorption is prevented, the patient is prescribed drugs from the group of disaccharides (Dufalac, Normase, Goodluck, Lizolac). Together with feces, the poisonous microelement quickly leaves the body.
In order to prevent cerebral edema in the early stages of the disease, hormonal systemic drugs Dexamethasone, Prednisolone are used. If the general condition worsens, the patient is hospitalized in the intensive care unit.
In case of hepatic encephalopathy against the background of acute liver failure, the patient is urgently referred for liver transplantation. An organ transplant will increase the chances of survival (statistics say about 70% of operated people who have overcome the five-year threshold). However, due to the high risk of complications and death, early consultation is required in a specialized medical center for the selection of donors and examination of the recipient.
Diet and diet
In acute liver encephalopathy, fasting for 1-2 days is recommended, after which the patient is prescribed a low-protein diet. With hepatic encephalopathy, the use of plant and animal proteins is limited to 0.5 g per 1 kilogram of body weight per day. In addition to protein products, salt is not allowed. To stabilize the condition, the patient is prescribed complexes of omega-3 fatty acids. With positive dynamics, the daily amount of protein is gradually increased. The volume is increased every five days by 5-10 g, but the maximum patient is allowed to eat no more than 50 g of low-fat dietary meat (rabbit, chicken, turkey).

It is worth noting that fasting in the early days of acute encephalopathy is not a prerequisite. If the patient's condition and analysis parameters are within acceptable values, it is enough to exclude protein products from the diet, giving preference to low-fat home-made food - soups, cereals, salads, pastries. In this case, you should pay attention to foods and drinks, the use of which is unacceptable in acute and chronic forms of the disease:
- apples, grapes, cabbage and other vegetables that cause intestinal fermentation;
- dairy products;
- whole milk;
- alcohol;
- sweet carbonated drinks;
- coffee;
- strong tea.
Hepatic encephalopathy with cirrhosis is accompanied by destructive changes in the organ. With the successful treatment of the disease, despite the ability of the liver parenchyma to recover quickly, one should constantly adhere to a diet to avoid relapse, since liver cells react sharply to the effects of harmful substances.
Chronic liver encephalopathy, therapy
In the chronic course of the disease, the principles of symptomatic therapy are adhered to. With an exacerbation of the disease, it is immediately necessary to adjust the diet and switch to a low-protein diet.
As with the acute form of hepatic encephalopathy, treatment involves the removal of toxic elements from the body. Most often, a two-stage bowel cleansing with medications that reduce the degree of ammonia concentration in the blood is required. To provide the patient with energy, a glucose solution is administered intravenously. In combination with the use of drugs, hepatic encephalopathy is treated with plasmapheresis procedures.
What are the chances that patients predict
The success of treatment depends largely on the severity of the patient's condition. , , . , , , .
25%, – 60%. . , .
, . 10 40 .