In modern conditions of environmental degradation, an increasingly terrible word sounds - oncology. Among all types of cancer, myeloma takes a special place. The etiology of this disease today raises more questions than answers. What is this - myeloma, why it appears, who is at risk - this article is about it .
There are many names, one essence
Myeloma (from the Greek myelos - brain) is a systemic lesion of the body associated with the cells of the hematopoietic system - the precursors of B-lymphocytes, which are capable of differentiation into plasma cells. According to the International Classification of Diseases, it has the code C.90 - C.93, refers to chronic leukocyte leukemia. In various sources, myeloma is called myeloma, Rustitsky-Calera disease, multiple myeloma, generalized plasmacytoma. But whatever it is called, it is a malignant tumor of plasma cells, localized mainly in the bone marrow. Normally, the bone marrow produces a certain number of plasmocytes. With the development of the disease, their number increases, and the formation of normal blood cells (white blood cells, red blood cells) decreases. Instead of antibodies that are responsible for immune defense, defective proteins are produced.
Statistics and reasons
Of the neoplasms of plasma cells, myeloma is the most common and accounts for up to 10% of all malignant blood diseases. Most patients are men over the age of 45. The main peak of myeloma is in the category of patients aged 65 to 70 years. In children, this pathology is not diagnosed.
The etiology of the disease remains unclear. Analysis of the patient’s history does not reveal toxic effects and antigenic stimulations.
Microbiology of the process
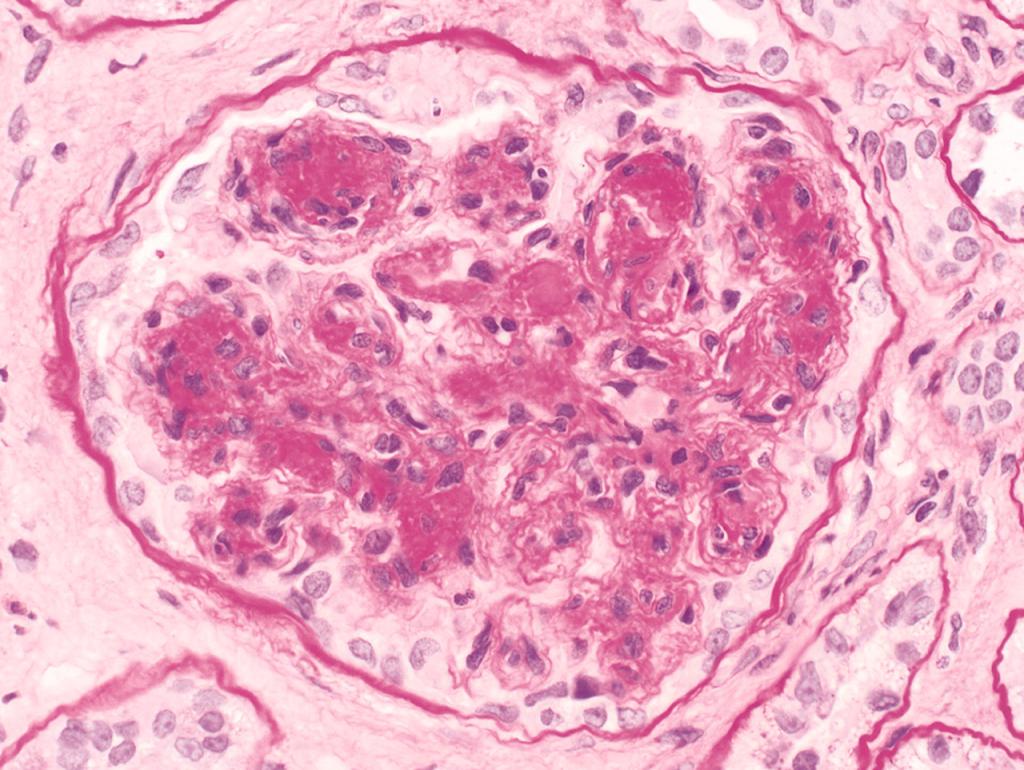
Plasma cells (plasmocytes) are cells that provide our immunity. They produce antibodies - the main proteins in the body's fight against pathogens. They are formed from the precursors of B-lymphocytes, and this happens in the bone marrow, lymph nodes and intestines. In a healthy person, plasmocytes make up 5% of the cells contained in the bone marrow. If their number becomes more than 10%, they talk about the development of myeloma (photo below - plasmocytes are painted in a darker color).
The process of plasmocyte formation consists of six stages, and only at the last stage of differentiation do lymphocytoplasmic cells acquire the ability to secrete antibodies (immunoglobulins) that can withstand various pathogens (viruses and bacteria). Thus, a normal plasmocyte is a unicellular gland of the immune system that secrets hundreds of antibodies per second.
How myeloma develops
At one of the six stages of plasmocyte formation, a malfunction can occur, and instead a myeloma cell with malignant properties, which consist in its continuous division, is formed. The accumulation of these cells, formed by dividing the original, is called plasmacytoma. It grows into bones or muscles, can be single or multiple. Myeloma cells themselves do not enter the bloodstream, but they secrete a lot of paraprotein, a pathological immunoglobulin. It does not play any role in the processes of immune defense, but is deposited in the tissue. It is he who is found in diagnostic blood tests.
In addition to paraproteins, such plasmocytes secrete special proteins - cytokines. These protein molecules stimulate the growth of malignant cells, inhibit immunity, activate osteoclasts - bone destroyers, activate the growth of fibroblasts (they increase blood density and lead to bruising and bruising), disrupt protein metabolism, which leads to damage to the kidneys and liver. In bone tissue, myeloma plasmocytes provoke destruction of cartilage and bone tissue, voids form in it.
Classification
This disease is a cancer of plasma cells, the result of which is the inability of the body to resist pathogens and problems of the circulatory system. By the nature of the spread of the tumor in the bone marrow, diffuse, diffuse-nodal and multiple-nodular forms of the disease are distinguished. According to the cellular composition of myeloma, there are plasmacytic, plasmoblast, polymorphic-cell, small-cell. Depending on the type of paraproteins that secrete myeloma plasmocytes, there are the following forms of the disease: non-secreting myelomas, diclone, Bens-Jones myeloma and G, A, M myelomas.
Risk groups
The causes of myeloma are not clear, but there are certain factors that increase the likelihood of the disease:
- Men over 40 years old. It is believed that with a decrease in the level of sex hormones in men, the risk of myeloma increases. Women rarely get sick.
- Genetic predisposition. 15% of patients had relatives who had this disease.
- Excess weight. Metabolic disorders in obesity reduce the body's immune status and create conditions for the development of malignant cells.
- Radiation and toxins. People who underwent radiation therapy, liquidators of the Chernobyl accident and those who are exposed to prolonged exposure to asbestos, arsenic are more likely to mutate B-lymphocytes. Some studies report similar effects of nicotine and alcohol.
- People with immunity pathologies - HIV-infected and taking medications that suppress the immune response.
- People with black skin are two times more likely to get sick than representatives of the Caucasian and Asian races.
Symptoms of Myeloma
While there are not very many myelin cells, the disease can be asymptomatic. With an increase in their number, they replace normal cells in the bone marrow, and more and more paraproteins enter the bloodstream. In myeloma, the symptoms appear primarily on the part of bone tissue, kidneys and the immune system. Moreover, the clinical picture depends on the stage of tumor development and the amount of paraproteins in the blood. In 10% of patients, abnormal cells do not produce defective proteins, and the disease proceeds without symptoms. In the clinical picture of myeloma blood disease prevail:
- General weakness and constant fatigue.
- Dramatic weight loss.
- Pain in bones and muscles. Headache.
- Pathological bone fractures.
- Immune status disorders, frequent infectious diseases.
- Increased blood viscosity and high ESR over a long period.
- Trophic lesions of the lower extremities not associated with varicose veins.
- Hemorrhages in the sclera of the eyes, bleeding gums, subcutaneous hemorrhages and bruises.
- Kidney damage.
What happens to bones
In most clinical cases, axillary resorption of bone tissue with the formation of cavities is observed. Sometimes there is smooth or lacunar resorption of the tissue. With the destruction of bones in the kidneys, lungs and blood vessels, phosphorus-calcareous masses are deposited as a metastasis. In the areas of micro-fractures, focal neoplasms of bone substance - osteosclerosis can form.
Together with the bone marrow, focal or diffuse infiltrates are found in the lymph nodes, tonsils, spleen and liver. In severe cases, there is an infiltration of these organs, their increase, nodal growths. Such manifestations of myeloma bring its manifestations closer to severe leukemia and complicate treatment, exacerbating the prognosis of the course of the disease.
Clinical stages of the disease
It is believed that from the moment of formation of the first tumors to the onset of symptoms of the disease, up to 15 years pass. During myeloma, two stages are distinguished:
- Benign stage. It is characterized by somatic compensation, a slow increase in bone pathology, moderately reduced blood counts, intact immunoglobulin titer, and a slow increase in paraprotein levels. The prognosis of treatment in this period is often favorable.
- Terminal stage. This is a period of acute inhibition of normal blood formation, the appearance of anemia, leukemia, thrombocytopenia. The level of normal antibodies drops sharply, until they are completely replaced with paraproteins. Metastasis with the formation of nodes in various organs with a feature of aggressive tumor growth indicates the transition of the disease to malignant sarcoma. The prognosis of the course of the disease is not so favorable.
Which doctor should I contact
A hematologist is involved in the diagnosis of myeloma. The determination is often difficult due to the general nature of the patient's complaints and the absence of symptoms in the initial stages. The diagnosis is clarified on the basis of additional studies:
- Clinical blood test. Myeloma is characterized by an increase in the viscosity and erythrocyte sedimentation rate (ESR), a decrease in the number of platelets and red blood cells, and a low hemoglobin content.
- Blood test for electrolytes. In myeloma, tests show an increase in calcium levels. Blood biochemistry is characterized by a high content of total protein, high numbers of urea and creatinine.
- Analysis of blood levels of paraproteins or abnormal antibodies.
- In urine tests, pathological chains of immunoglobulins (Bens-Jones proteins) are found.
- A bone x-ray shows cavities characteristic of myeloma. Computed tomography, MRI, and PET scans will show the same damage.
- The most reliable way to diagnose myeloma is sternal bone marrow puncture. It is taken from the sternum or pelvic bones, examined under a microscope in order to determine myeloma plasmocytes.
The treatment is complex and lengthy.
After diagnosing myeloma, treatment is carried out in a hospital setting. Used complex drug therapy, including:
- Targeted therapy with drugs that affect protein synthesis and lead to the death of plasmocytes (for example, the drug "Karfilzomib").
- Biotherapy is aimed at stimulating the immune system (for example, Thalidomide or Lenalidomide).
- Chemotherapy is aimed at inhibiting tumor growth and the death of pathological cells (Cyclophosphamide and Melphalanum).
- Corticosteroid therapy is used as an adjunct.
- To increase the density of tissues, bisphosphonates (Pamidronate) are prescribed.
- Analgesics are used if necessary to relieve pain.
If necessary, surgery is performed. For example, if it is necessary to fix the vertebrae when bone fractures are revealed.
Perhaps the use of bone marrow transplantation. In this case, bone marrow stem cell transplantation of the patient himself is more often used.
It is important to comply with all doctor's prescriptions and strictly adhere to the schedule of control checks. Then the prognosis of myeloma can be favorable.
Associated complications
As with any systemic disease, in this case, the complications may be as follows:
- Very strong pain that requires high-quality anesthesia.
- Renal failure, up to the need for hemodialysis.
- Frequent and prolonged infectious diseases.
- Pathological fractures due to thinning of bone tissue.
- Anemia requiring a blood transfusion.
Myeloma and prognosis
The treatment of myeloma is much more optimistic today than 20 years ago. On average, out of 100 patients, 77 will live another year, and 23 will live at least 10 years. The so-called "smoldering" myeloma, which does not progress and is almost asymptomatic for many years, requires regular medical examinations and monitoring the development of the disease. Early diagnosis of activation of bone destruction and proper therapy make prognoses the most favorable.
A fatal outcome most often occurs as a result of infectious complications, critical blood loss, severe renal failure, and pulmonary embolism.
Prevention and recommendations
Myeloma is unpredictable and insidious. Therefore, special prevention does not exist. There are studies that show a correlation between a healthy and active lifestyle in old age and a reduced risk of disease. In the initial stages of the development of the disease, patients are advised to adhere to certain nutritional rules, namely:
- Exclude canned foods and convenience foods from the diet.
- Increase the amount of foods rich in iron - bell peppers, red meat, broccoli, papaya, mango.
- Include more fruits and vegetables in your diet.
- Reduce the intake of protein foods, including milk and dairy products, eggs, beans, nuts.
There are studies on the beneficial effects of oriental turmeric. The antioxidant curcumin contained in it has anti-inflammatory properties and helps to slow down the growth of tumor cells, as well as prevents resistance to chemotherapy drugs.
What does traditional medicine advise
Alternative methods of treating the disease are divided into two groups:
- Therapy based on the intake of infusions of poisonous plants (hemlock, fly agaric, celandine), which is aimed at slowing the growth of tumors. These plants contain alkaloids similar to chemotherapy. Reception of such funds should be very accurate - exceeding the dosage can lead to severe poisoning and even death. It is better to discuss a dosage with the doctor.
- Reception of infusions aimed at improving the immune status and general condition of the patient. Apply infusions based on the marsh cinquefoil, Melilotus officinalis, officinalis Veronica, meadowsweet, comfrey, milkweed. These funds will not be able to defeat the disease, but they can improve the quality of life and overall well-being of the patient.
It is desirable to apply the means of the first and second groups in a complex. At the same time, remedies based on poisonous plants are used in courses with mandatory interruptions. And any remedy should not be used for more than a month, in order to avoid getting used to the body and losing the healing effect. In any case, before using traditional drugs, you should consult your doctor. Modern medicine is far from being as conservative as we are used to thinking and is ready to consider all options for a favorable prognosis of myeloma.