The word "leper" even in our time is endowed with sharply negative subtext. The concept of "leprosy" for many is, although not entirely clear, but very unpleasant, but before it was terrifying and horrifying for everyone. In this article we will tell you what kind of ailment it is - leprosy, what are its symptoms, etiology, epidemiology, pathogenesis, what treatment is there, and most importantly, whether leper people need to be afraid, and how you can get infected from them.
Leprosy or leprosy?
There is a disease in which the face becomes incredibly repulsive, and the hands and feet become ugly due to the loss of fingers. She has about a dozen names. There are exotic ones - a mournful disease, a Phoenician disease, lazy death. There are sophisticated ones, for example, hansenosis or chronic granulomatosis, but there are widely known ones, such as leprosy or leprosy, which gave rise to the terrible word “leper”. Each name emphasizes one or another feature of the ailment. For example, “hansenosis” appeared in honor of the scientist Hansen, who first discovered the causative agent of the disease, and “leprosy” came from the ancient Greek lepras, that is, “scales”. Apparently, she was reminded by the ancient Greeks of growths and terrible scabs on the faces of patients. The ancient Slavs, on the basis of the words “about” and “KaziT”, that is, changing their appearance, called the sore “leprosy”. Etiology, pathogenesis, and even more so the treatment of the disease still cause controversy and disagreement, and before people knew absolutely nothing about it, so they were afraid. The Church declared the disease punishment of the Lord for transgressions, and believers did not dare to doubt it. So it became the only method of treatment for the supplication of sins.

A few historical facts
Scientists conducted a series of analyzes of ancient remains and found that for more than 6 thousand years, humanity has known horror by the name of leprosy. The etiology and pathogenesis of the disease were described by Hippocrates, but he mistakenly attributed psoriasis there too. Africa is considered to be the birthplace of leprosy (according to other sources, Asia, hence the Phoenician disease), “valiant” crusaders brought infection to Europe, and its discoverers and their followers to America. Having received a huge number of fresh victims and without encountering obstacles, the disease easily conquered half the world. No one had a clue, leprosy - what is it. The etiology and pathogenesis of leprosy came down to the fact that a person suddenly became a freak, his fingers and toes fell off, and then he himself rotted alive. People were in panic and in every way got rid of lepers. At best, they were simply expelled. There was a ritual of the "funeral" of the unfortunate, during which he was put in a coffin, boarded up, lowered into a pit and even sprinkled with earth. After that, it’s true, they got it, but for all, man no longer existed among the living. In the worst case, the patient was killed for real. How it would end is unknown, but the incredible happened - Europe was attacked by another deadly infection that supplanted the first. After the plague pandemic, leprosy became a rare occurrence here.
Leprosy today
Back in the Middle Ages, monasteries created houses for lepers, where they lived until their death. They called them leprosoria. In 1873, the scientist Hansen, who worked in one of these institutions, managed to find bacteria unprecedented in material taken from a patient. They were called Hansen's wands. But many more years passed before they figured out their connection with a disease such as leprosy. The etiology, pathogenesis, and treatment methods are now more understood. Once upon a time there were thousands of leper colony in the world, because then there were more than 20 million lepers. In Russia alone, there were 19 leprosoria. Thanks to the medicine found, by the end of the 20th century the number of patients in the world decreased to 12 million, and at the moment there are about one and a half million. However, statistics for 2015 again showed a slight increase in the number of patients. There are only 4 leprosoria in Russia, and 600 people with leprosy. The bulk of the “lepers” is now concentrated in India, China, and other countries of South Asia, almost throughout Africa, including Madagascar, in South America, on the Arabian Peninsula, in the Philippines, in the Caribbean.

Pathogen portrait
The pathogenesis of leprosy begins with the penetration of Hansen's sticks into the human body. It is a microscopic bacterium up to 8 microns long and only 0.5 microns in diameter. The sticks have sharpened or thickened edges and are covered with four layers of very dense shells that protect them from external stimuli. They are motionless, do not form spores, reproduce incredibly slowly. The division of one bacterium lasts approximately 14 days. Sticks are held in groups, then they resemble spilled cigarettes. Sometimes parasites can be found one at a time. They live exclusively in the cells of the victims, therefore, once in the external environment, they quickly die. Hansen’s sticks are only parasitic in humans, but it is believed that they can infect mice, armadillos, chipmunks and some species of monkeys. The etiology and pathogenesis of leprosy (leprosy) is difficult to study, because the colonies of Hansen's rods on a nutrient medium in laboratories grow unusually poorly and slowly - from 6 weeks, versus several hours in other bacteria. Another difficulty is that they become non-pathogenic outside the cell, and practically do not take root in experimental animals. Nevertheless, it was possible to find out that Hansen and Koch bacilli (cause tuberculosis) came from one bacterium, but in the process of evolution they altered their structures somewhat. And in 2009, another species of this bacterium was discovered, which causes diffuse lepromatous leprosy.

Infection pathways
The source of the microbe of leprosy can only be a person suffering from this ailment in an active form. But according to some reports, sometimes the cause of infection becomes work without gloves with animals that are affected by the Hansen bacterium. How is the pathogenesis of leprosy? Airborne infections are always the most virulent and can infect many. But in the case of leprosy, this does not happen for reasons as yet unclear. It is only known that Hansen's sticks actively multiply in areas of the body that can cool the air, namely in the mucous membranes of the oral cavity. From a sick person to healthy they are transmitted by sneezing, kissing, coughing, emotional conversation. In addition, the microbe can be transmitted with the blood of the patient or when his exudates, saturated with parasites, get directly onto the injured skin of the new victim.
Risk groups
Those in whose families have leprosy are highly likely to become infected. Firstly, due to the fact that it is difficult to avoid long contacts between family members, and secondly, because there is a genetic predisposition to this disease. Couples are forbidden to have heirs. But in sick mothers, children are born healthy. If these babies are immediately isolated, they are not completely affected by leprosy (leprosy). The etiology of the disease has not yet been clarified in relation to other risk categories among the population. It has so far been established that the disease is actively developing in people with weakened immunity. There are cases when people caring for lepers remained healthy, but their relatives who did not participate in the care fell ill. The doctor Daniel Danielson injected the blood of lepers for many years, put exudate from the tubercles on their body into his wounds, but was never infected. In general, the disease is most likely where there is a low standard of living.

Pathogenesis of leprosy
Presumably, due to the slow multiplication of Hansen bacteria, the leprosy caused by them develops too long. The etiology and pathogenesis of the disease are as follows: the pathogen, having got on the mucous membranes or in the wound, seeps into the blood and lymph, and with these fluids into the nervous system and other internal organs. There, bacteria form granulomas containing many macrophages. Having become infected, a person can live for decades and not suspect about his illness. The incubation period in some lasts for six months, usually about 5 years, and in some cases 20 or even 40 years. In addition to the incubation period, there is a latent period (the time from which the infected person is able to infect others). For leprosy, it is slightly less than incubation. The patient at this time may have no symptoms at all, or there may be slight malaise, loss of appetite, inexplicably fatigue, but he does not suggest a serious illness, although it is already contagious.
Symptoms
The microbe affects not only the mucous membranes in the mouth, but also in the lungs, as well as cells in the nerve endings (Schwanowski). With the progression of the disease, bacteria are found in the eyes, in the liver, even in the brain. The first sign of an ailment is severely tolerated pain in the limbs, in the back. Then patients can complain of weakness, drowsiness, loss of appetite, and intestinal upset. In the future, pain is replaced by a tingling sensation, and then the person generally loses sensitivity in the affected areas. This often causes injuries, infection with another infection, and ultimately loss of fingers, irreversible defects in the arms and legs. Hansen's sticks alone do not deprive a sick limb. In leprosy, two main types are distinguished - tuberculoid leprosy and lepromatous. Their symptoms are different, so consider each in more detail.
Tuberculoid leprosy, etiology, symptoms, treatment
This type of disease is diagnosed in three forms:
- polar;
- borderline;
- undifferentiated.
The main symptom of tuberculoid leprosy is the appearance on the skin of a clear hypopigmented (light) spot. The undifferentiated form is able to heal on its own, or go to more severe ones. At first, the skin at the site of pigmentation is very sensitive, but soon the stain begins to increase, its edges protrude, and the central part, on the contrary, sinks. There are no sweat glands, hair disappears, the skin loses its sensitivity. Outside the spot, the nerves thicken, as Hansen's sticks, expanding, inflate the affected cells. Nerve infection causes muscle atrophy, contracture of the feet and hands. When bacteria infect the facial nerve, patients develop eye diseases that ultimately lead to blindness.
Lepromatous leprosy
This type of disease is more severe and more dangerous for people around the patient. Two forms are distinguished here:
Spots are also one of the primary symptoms of the disease, but they have a slightly different picture - they are extensive, arranged symmetrically with respect to the conditional midline of the human body, with fuzzy borders and a dense convex center. In addition to spots, rashes can take the form of nodules, plaques or papules. All of them are called leprosy and contain thousands of Hansen sticks in the infiltrate. It is very characteristic what happens during leprosy with the faces of patients. Their eyelashes and eyebrows fall out, their nose falls off (late stages), the shape of the ears is distorted (thickens), the skin on their faces (the “lion's face”), facial expressions are broken. Other symptoms:
- problems with the nose (nasal congestion, difficulty breathing, sometimes blood comes from the nose);
- voice change (becomes hoarse);
- vision problems (keratitis, iridocyclitis);
- enlarged lymph nodes in the groin;
- testicular tissue infiltration;
- the formation of disfiguring ulcers in place of leprosy disintegrated;
- weakness of the limbs, atrophy, and later necrosis.
There is a mixed form of leprosy, in which symptoms of tuberculoid and lepromatous forms are simultaneously observed.
Diagnostics
The disease of leprosy, the etiology and pathogenesis of which is still being studied, is diagnosed by several methods.
- Clinical. It consists in a visual examination of the patient's skin, identifying insensitive mucous membranes and skin areas.
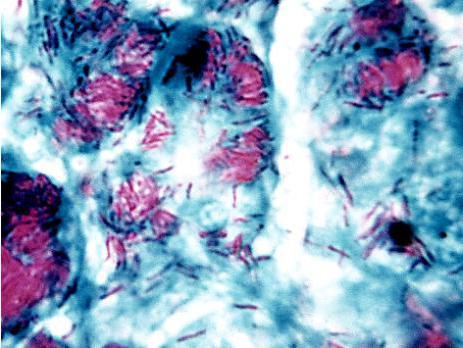
- Microscopic. In the nasopharynx, a rather intense (to the blood) scraping is done, material is taken from the lymph nodes. The microscope shows the patient the presence of characteristic oval or round leprosy cells. Smears are stained according to the Ziehl-Nielsen method, as a result, old Hansen sticks turn red, and young ones are mostly blue.
- Allergic test (Mit-trial). Lepromin is injected under the skin (prepared from tissues taken from patients with leprosy). If the test subject is infected, his skin swells and turns red at less than one day in the sample.
- Serological method.
Treatment
Leprosy is treated for a very long time, up to 12 months, and sometimes several years. Therapy is only complex with the participation of ophthalmologists, orthopedists, neuropathologists. Antibacterial drugs are also used in combination. This is Dapson in tandem with Clofazimine and Rifampicin. For each patient, the dose and the algorithm for taking medications are individual. Some forms of the disease can be treated with only two of the three antibiotics given, as determined by the doctor. Currently, tests are being conducted on the medicines Minocycline, Clarithromycin, Ofloxacin as anti-leprosy medicines. As a result, all leprosy bacteria are killed in patients, but the damage they cause to organs and skin (if it comes to that) remains.
Forecast
If treatment is started on time, the outcome is quite favorable. Patients may not even have any marks on their skin. In the advanced stages, it is no longer possible to restore health, a person remains disabled for life, but he can restore the work of internal organs, which allows him to extend his life.
Disease prevention includes:
- hygiene, especially when located in regions where leprosy thrives;
- early diagnosis and treatment;
- preventive control of all those who have long contacts with patients with leprosy (doctors, family).