Antibiotics are a group of drugs with an etiotropic mechanism of action. In other words, these drugs act directly on the cause of the disease (in this case, the pathogen microorganism) and do it in two ways: they destroy the microbes (bactericidal drugs - penicillins, cephalosporins) or prevent their reproduction (bacteriostatic - tetracyclines, sulfonamides).
There are a huge number of drugs that are antibiotics, but the most extensive group among them is beta-lactams. It is about them that will be discussed in this article.
Classification of antibacterial agents
According to the mechanism of action, these drugs are divided into six main groups:
- Antibiotics that disrupt the synthesis of components of cell membranes: penicillins, cephalosporins, etc.
- Medicines that interfere with the normal functioning of the cell wall: polyenes, polymyxins.
- Drugs that inhibit protein synthesis: macrolides, tetracyclines, aminoglycosides, etc.
- Suppressing RNA synthesis at the stage of action of RNA polymerase: rifampicins, sulfonamides.
- Suppressing RNA synthesis at the stage of DNA polymerase action: actinomycin, etc.
- DNA synthesis blockers: anthracyclines, nitrofurans, etc.
However, this classification is not very convenient. In clinical practice, the following separation of antibacterial drugs is accepted:
- Penicillins.
- Cephalosporins.
- Macrolides.
- Aminoglycosides.
- Polymyxins and polyenes.
- Tetracyclines.
- Sulfonamides.
- Derivatives of aminoquinolones.
- Nitrofurans.
- Fluoroquinolones.
Beta-lactam antibiotics. The structure and mechanism of action
This is a group of drugs with a bactericidal effect and a fairly wide list of indications for use. Beta-lactam antibiotics include penicillins, cephalosporins, carbapenems, monobactams. All of them are characterized by high efficiency and relatively low toxicity, which makes them the drugs most often prescribed for the treatment of many diseases.
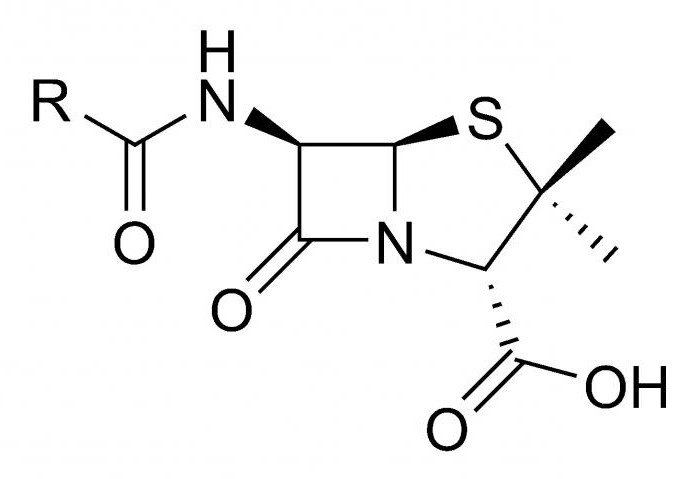
The mechanism of action of beta-lactam antibiotics is due to their structure. Excessive details are useless here, it is worth mentioning only the most important element, which gave the name to the entire group of drugs. The beta-lactam ring that is part of their molecules provides a pronounced bactericidal effect, which is manifested by blocking the synthesis of elements of the cell wall of the pathogen. However, many bacteria can produce a special enzyme that violates the structure of the ring, thereby depriving the antibiotic of its main weapon. That is why the use in the treatment of drugs that do not have protection against beta-lactamases is ineffective.
Beta-lactam antibiotics, which are protected from the action of a bacterial enzyme, are becoming increasingly common. They include substances that block the synthesis of beta-lactamases, for example, clavulonic acid. This is how protected beta-lactam antibiotics are created (such as Amoxiclav). Other bacterial enzyme inhibitors include Sulbactam and Tazobactam.
Penicillin Medicines: A Historical Background
Drugs of this series were the first antibiotics, the therapeutic effect of which became known to people. For a long time they were widely used to treat various diseases and in the first years of use were almost a panacea. However, it soon became clear that their effectiveness was gradually falling, since the evolution of the world of bacteria does not stand still. Microorganisms are able to quickly adapt to a variety of complex living conditions, giving rise to the generation of antibiotic-resistant bacteria.
The prevalence of penicillins has led to the rapid growth of microbial strains insensitive to them, therefore, in its pure form, preparations of this group are now ineffective and almost never used. They are best used in combination with substances that enhance their bactericidal effect, as well as inhibit the protective mechanisms of bacteria.
Penicillin preparations
These are beta-lactam antibiotics, the classification of which is quite extensive:
- Natural penicillins (for example, "Benzylpenicillin").
- Antistaphylococcal ("Oxacillin").
- Extended-action penicillins (Ampicillin, Amoxicillin).
- Antiseptic ("Azlocillin").
- Protected penicillins (combined with clavulonic acid, Sulbactam, Tazobactam).
- Drugs that include several penicillin antibiotics.
Brief review of penicillin drugs
Natural penicillins can successfully suppress the activity of both gram-positive and gram-negative microorganisms. Of the latter, streptococci and the causative agent of meningitis are the most sensitive to this group of beta-lactam antibiotics. The remaining bacteria have now acquired protective mechanisms. Natural penicillins are also effective against anaerobes: clostridia, peptococci, peptostreptococci, etc. These drugs are the least toxic and have a relatively small number of undesirable effects, the list of which comes down mainly to allergic manifestations, although with an overdose it is possible to develop a convulsive syndrome and the appearance of symptoms of poisoning with side of the digestive system.
Of the anti-staphylococcal penicillins, beta-lactam antibiotic such as Oxacillin is of greatest importance. This drug is for narrow use, as it is intended primarily to combat Staphylococcus aureus. It is against this pathogen (including penicillin-resistant strains) that Oxacillin is most effective. Side effects are similar to those of other representatives of this group of drugs.
Extended-spectrum penicillins, in addition to gram-positive, gram-negative flora and anaerobes, are also active against intestinal pathogens. Side effects do not differ from the above, although these drugs are characterized by a slightly higher probability of disorders of the digestive system.
Beta-lactam antibiotic "Azlocillin" (representative of the fourth group of penicillins) is designed to combat Pseudomonas aeruginosa. However, at present, this pathogen has shown resistance to drugs of this series, which makes their use not so effective.
Protected penicillins have already been mentioned above. Due to the fact that these drugs include substances that suppress beta-lactamase bacteria, they are more effective in treating many diseases.
The last group is a combination of several representatives of the penicillin series, mutually reinforcing the effect of each other.
Four generations of bacteria destroyers
Cephalosporins are also beta-lactam antibiotics. These drugs, like penicillins, are distinguished by the breadth of the spectrum of action and the insignificance of side effects.
There are four groups (generations) of cephalosporins:
- The most prominent representatives of the first generation are Cefazolin and Cephalexin. They are intended primarily to combat staphylococci, streptococci, meningococci and gonococci, as well as some gram-negative microorganisms.
- The second generation is the cefuroxime beta-lactam antibiotic. His area of responsibility includes mainly gram-negative microflora.
- "Cefotaxime", "Ceftazidime" - representatives of the third group of this classification. They are very effective against enterobacteria, and are also able to destroy nosocomial flora (hospital strains of microorganisms).
- The main drug of the fourth generation is Cefepim. It has all the advantages of the above medicines, in addition, it is extremely resistant to the action of beta-lactamase bacteria and has activity against Pseudomonas aeruginosa.
Cephalosporins and beta-lactam antibiotics are generally characterized by a pronounced bactericidal effect.
Of the undesirable reactions to the administration of these drugs, the most attention is paid to a variety of allergic reactions (from minor rashes to life-threatening conditions, such as, for example, anaphylactic shock), in some cases digestive disorders are possible.
Backup tool
Imipenem is a beta-lactam antibiotic belonging to the carbapenem group. He, as well as the equally well-known "Meropenem", in terms of the effectiveness of its effect on microflora resistant to other drugs, can give odds even to the third and fourth generations of cephalosporins.
A beta-lactam antibiotic from the carbapenem group is a drug used in especially severe cases of diseases when pathogens cannot be treated with other drugs.
Backup facility number two
"Aztreonam" is the most striking representative of monobactam, it is characterized by a fairly narrow spectrum of action. This beta-lactam antibiotic is most effective against gram-negative aerobes. However, it should be noted that, like Imipenem, Aztreonam is practically insensitive to beta-lactamases, which makes it the drug of choice for severe forms of diseases caused by these pathogens, especially when treatment with other antibiotics is ineffective.
Beta-lactam antibiotic spectrum
Summarizing the above, it should be noted that the preparations of these groups affect a huge number of varieties of pathogens. The mechanism of action of beta-lactam antibiotics is such that there is no chance for microbes to survive: the blockade of cell wall synthesis is a death sentence for bacteria.
Gram-positive and gram-negative organisms, aerobes and anaerobes ... On all these representatives of the pathogenic flora there is a highly effective drug. Of course, among these antibiotics there are also highly specialized drugs, but most of them are still ready to engage in battle with several pathogens of infectious diseases at once. Beta-lactam antibiotics are able to withstand even representatives of the nosocomial flora, which is the most resistant to treatment.
What are hospital strains?
We are talking about microorganisms existing in medical institutions. The sources of their appearance are patients and medical staff. Hidden, sluggish forms of disease are especially dangerous. The hospital is an ideal place where carriers of all possible types of infectious diseases gather. And violations of sanitary rules and norms are fertile ground for this flora to find a niche for itself to exist, where it can live, reproduce and become resistant to drugs.
The high resistance of hospital strains is due primarily to the fact that, having chosen a hospital facility as their habitat, bacteria are able to contact with various drugs. Naturally, the effect of drugs on microorganisms occurs randomly, with no purpose to destroy, and in small doses, and this contributes to the fact that representatives of hospital microflora can develop protection against mechanisms that are harmful to them, learn to resist them. So there are strains that are very difficult to fight, and sometimes it seems impossible.
Beta-lactam antibiotics to one degree or another try to solve this difficult problem. Among them are representatives who are able to quite successfully fight even the most drug-insensitive bacteria. These are reserve drugs . Their use is limited, and they are appointed only when it is really necessary. If these antibiotics are used unreasonably often, then most likely it will end with a drop in their effectiveness, because then the bacteria will be able to interact with small doses of these drugs, study them and develop ways of protection.
When are beta-lactam antibiotics prescribed?
Indications for use of this group of drugs are primarily due to their spectrum of action. It is most advisable to prescribe a beta-lactam antibiotic for infection, the causative agent of which is sensitive to the action of this drug.
Penicillins have proven themselves in the treatment of pharyngitis, tonsillitis, pneumonia, scarlet fever, meningitis, bacterial endocarditis, actinomycosis, anaerobic infections, leptospirosis, salmonellosis, shigellosis, infectious diseases of the skin and soft tissues. Do not forget about drugs that can fight Pseudomonas aeruginosa.
Cephalosporins have a similar spectrum of action, therefore, the indications for them are almost the same as for penicillins. However, it should be said that the effectiveness of cephalosporins, especially the last two generations, is not an example higher.
Monobactams and carbapenems are designed to combat the most severe and poorly treatable diseases, including those caused by hospital strains. They are also effective in sepsis and septic shock.
Unwanted action
As already mentioned, beta-lactam antibiotics (drugs belonging to this group are listed above) differ in a relatively small number of effects harmful to the body. Rarely occurring convulsive syndrome and digestive system symptoms do not pose a threat to life. Severe allergic reactions to the administration of beta-lactam antibiotic drugs can be truly dangerous.
Rashes, pruritus, rhinitis and conjunctivitis do not pose a threat to life, although they are very unpleasant. What you should really be afraid of is severe reactions such as Quincke's edema (especially in the larynx, which is accompanied by severe suffocation up to the inability to breathe) and anaphylactic shock. Therefore, the drug can be administered only after performing an allergy test.
Cross reactions are also possible. Beta-lactam antibiotics, the classification of which implies the presence of a large number of groups of drugs, are very similar in structure to each other, which means that if one of them is intolerant, all the others will also be perceived by the body as an allergen.
A few words about the factors that increase the resistance of bacteria
A gradual decrease in the effectiveness of antibacterial drugs (including beta-lactam antibiotics) is due to their unreasonably frequent and often incorrect prescription. An incomplete course of treatment, the use of small therapeutic doses do not contribute to recovery, but give microorganisms the opportunity to "train", invent and develop methods of protection against drugs. So is it any wonder that the latter become ineffective over time?
Although antibiotics are not currently available in pharmacies without a prescription, you can still get them. This means that self-medication and the problems associated with it (using the same drug all the time, unreasonable interruption of the course of therapy, improperly selected doses, etc.) will remain, creating the conditions for the cultivation of resistant strains.
The hospital flora, which has the ability to actively contact with various drugs and invent new ways to counter them, will not go anywhere.
What to do? Do not self-medicate, follow the recommendations of your doctor: take the medicine for as long as required, and in the right doses. Of course, it is more difficult to deal with nosocomial flora, but still it is possible. Tightening sanitary standards and their strict implementation will reduce the likelihood of creating favorable conditions for the propagation of resistant flora.
A few words in conclusion
A very broad topic is beta-lactam antibiotics. Pharmacology (the science of drugs and their effect on the body) devotes several chapters to them, which include not only the general characteristics of the group, but also contain a description of its most famous representatives. This article does not claim to be complete, it is only trying to introduce you to the main points that you simply need to know about these drugs.
Stay healthy and do not forget: before using this or that antibiotic, carefully study the instructions and strictly follow the recommendations, and even better consult with a specialist.