Often, patients of general practitioners hear in response to their complaints a menacing diagnosis of lymphadenitis. What it is? Despite the extremely unpleasant manifestations of this infectious disease, it lends itself to conservative treatment and rarely causes complications. Lymphadenitis is an inflammation of the lymph nodes due to their infection with a virus or bacteria. In rare cases, the inflammatory process is the result of the growth of cancer cells.
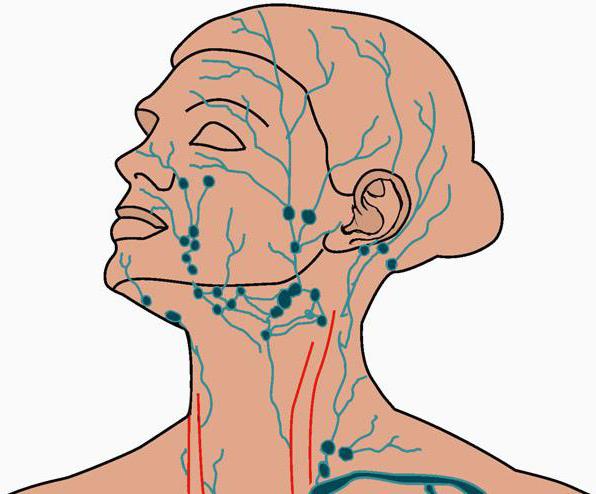
Lymph nodes are an essential element of the body’s immune system, designed to fight any pathogens of infections. Most often, they swell on the neck, under the chin, in the armpits, in the groin.
Sometimes for the treatment of inflammation it is enough just to wait and apply warm compresses to the sore spot from time to time. However, only a qualified doctor can accurately determine the method of therapy, since the effectiveness of treatment completely depends on the cause of swelling of the lymph nodes.
Symptoms
Lymphadenitis - what is it, an independent disease or a sign of a more serious condition? Sometimes inflammation of the lymph nodes occurs on its own, but in some cases it is a manifestation of another ailment. At the very beginning of the inflammatory process, the patient often notices that the lymph nodes became more sensitive, and touching them became painful. In addition, they can significantly increase and acquire the size of a pea or bean. In advanced cases, the lymph nodes become even larger.
Depending on the cause of inflammation, the following symptoms are distinguished:
- runny nose, sore throat, fever and other signs of an upper respiratory tract infection;
- general swelling of the lymph nodes throughout the body, which may indicate an infection (HIV or mononucleosis) or damage to the immune system (for example, ordinary lupus or rheumatoid arthritis);
- swelling of the extremity caused by clogging of the lymphatic system due to inflammation in the lymph node, located deep under the skin;
- hardened fixed fast-growing nodules, which serve as a sign of tumor development;
- fever;
- increased sweating at night.
When to see a doctor
If you find yourself with lymphadenitis, it is better to postpone treatment with folk remedies for later - it is better to immediately sign up for a medical consultation with a therapist who can make an accurate diagnosis and prescribe a really effective therapy.
Do not postpone a visit to the clinic if:
- inflammation makes you anxious;
- it began for no apparent reason;
- the inflammatory process continues to intensify or does not go away within 2-4 weeks;
- the lymph nodes feel firm or rubbery to the touch, or if they do not move when pressed;
- swelling of the lymph nodes is accompanied by constantly high body temperature, profuse sweating at night or unexplained weight loss;
- lymphadenitis is complicated by sore throat or difficulty swallowing or breathing.
Causes
The lymph node is a small, round or bean-like cluster of cells covered with a membrane of connective tissue. Cells are a group of lymphocytes (producing protein particles used to capture parasites - for example, viruses) and macrophages that destroy captured biological material. Lymphocytes and macrophages filter the lymph that flows through the entire body, and thereby protect the body from pathogens.
Lymph nodes are grouped in small groups, each of which is responsible for a specific part of the body. Most often, adult lymphadenitis is localized on the neck, under the chin, in the armpits or in the groin. The swollen area indirectly indicates the root cause of inflammation.
Most often, such unpleasant symptoms are accompanied by various infectious diseases - for example, such a common infection with the virus as a common cold. However, there are other types of infections, as well as other diseases that cause inflammation of the lymph nodes, including:
- acute pharyngitis;
- measles;
- ear infections;
- infection (abscess) of the tooth;
- mononucleosis;
- skin infections or open wounds (for example, cellulitis or erysipelas) ;
- human immunodeficiency virus (HIV) causing AIDS;
- tuberculosis;
- some sexually transmitted diseases, including syphilis;
- toxoplasmosis - a parasitic infection due to contact with the feces of an infected cat or eating poorly fried meat;
- benign viral lymphadenitis (what is it, if you do not know, then, perhaps, the name "cat scratch disease" will seem more familiar to you);
- lupus erythematosus - a chronic inflammatory disease that affects the ligaments, skin, kidneys, blood cells, heart and lungs;
- rheumatoid arthritis - a chronic inflammatory disease that affects the membrane of the joints (synovial membrane);
- lymphoma - a cancer that develops in the lymphatic system;
- leukemia - cancer of the hematopoietic tissue, also affecting the bone marrow and lymphatic system;
- other cancers that spread in the form of metastases to the lymph nodes.
In rare cases, serous lymphadenitis can be caused by taking certain medications - such as the anticonvulsant drug phenytoin (Diphenin, Dilantin) and drugs for the prevention of malaria.
Complications
If the cause of lymph node swelling was an infection, in the absence of adequate treatment, the following complications may develop:
- The formation of an abscess. An abscess is a localized accumulation of pus, a consequence of infection of the body with a virus or bacteria. Pus contains fluid, white blood cells, dead tissue, and bacteria. You may need to drain and start taking antibiotics to remove the abscess. It is especially dangerous if in any way it affects a vital organ.
- Bloodstream infection (bacteremia). A bacterial infection in any part of the body can lead to sepsis caused by infection of the bloodstream. Sepsis can cause dysfunction of vital organs and death. Treatment involves being in a hospital and administering antibiotics intravenously.
Before a visit to the doctor
When any potentially dangerous symptom is detected, people have many questions. Why are lymph nodes inflamed? Is it lymphadenitis? What is it - an infection or a sign of a more serious disease that requires early treatment? Exact answers to these and other questions can be obtained only from a qualified doctor. If you are only concerned about swelling in one part of the body, you should wait for the appointment at the clinic. If the manifestations of the inflammatory process become so intense that it is difficult for you to breathe or swallow, immediately call an ambulance.
Since medical consultations are significantly limited in duration and mean that the doctor will immediately give you a lot of new and extremely important information, get ready to visit a specialist in advance.
- When making an appointment, check if you need to do anything before visiting a doctor.
- Make a list of all your symptoms and indicate how long they last. Your doctor will probably want to know if you have any flu symptoms like fever or sore throat. In addition, the specialist will be interested in changes in body weight, which often accompany lymphadenitis. Reviews of your well-being over the past few days are mandatory - write down any signs of ailments that you began to notice since the lymph nodes first began to swell.
- Make a list of all the events during which you contacted potential sources of viruses and bacteria. This can be a trip abroad, a tourist trip to places teeming with ticks, eating poorly fried meat, playing with a domestic cat that ended up getting scratched, or having sex with unfamiliar partners without proper means of protection against infections.
- Write down all the important information regarding your health status, as this will help your doctor diagnose lymphadenitis. Treatment with folk remedies and traditional drugs, surgery, regular intake of dietary supplements, even ordinary vitamins - all this should be indicated.
- Think in advance about the questions you will need to ask your doctor. Just in case, it is worth ranking them, starting with the most important ones.
Questions to a specialist
If your serous lymphadenitis is progressing steadily, consider asking the therapist the following questions:
- What caused these symptoms?
- Could they be signs of another disease?
- What research do I need to go through?
- What treatment do you recommend?
- Will my condition improve soon?
- Is my disease contagious? How to reduce the risk of spreading the infection to other people?
- What preventive measures should be taken in the future to prevent a relapse of the disease?
- I suffer from chronic illnesses. Is there any need to change the therapy that I am currently following?
- You have prescribed me medicines. Are there alternative drugs?
- Can you recommend additional sources of information about this disease and its treatment?
- What to expect from a doctor
- Whether it is parotid inflammation or axillary lymphadenitis, treatment in any case will depend primarily on the root cause of the pathology. To determine this root cause, the doctor will first ask you a series of questions for which it is desirable to prepare answers in advance. These questions can be formulated as follows:
- What symptoms did you notice at home?
- When did the signs of pathology first appear?
- Do lymph nodes increase over time?
- What are inflamed lymph nodes to the touch?
- Do you suffer from fever (fever) or night sweats?
- Do you monitor your weight? Do you lose weight without trying to lose weight?
- Do you have a sore throat? Is it hard to swallow?
- Do you have any difficulty breathing?
- Has your bowel and bladder changed?
- What medications are you currently taking? Are you trying to treat lymphadenitis on your own? Do compresses help or have no effect?
- Have you recently traveled to foreign countries or to regions where ticks live? Are your fellow travelers sick?
- Have you been in contact recently with unfamiliar or unfamiliar animals? Did they suffer from bites or scratches?
- Have you recently had contact with a new sexual partner?
- Do you practice safe sex?
- Do you smoke? If so, for how many years?
Before diagnosis
While you are waiting for an appointment, axillary or parotid lymphadenitis can be treated with warm compresses. If necessary, take painkillers such as ibuprofen or paracetamol (Tylenol, etc.). Similar drugs are also available for children, and a prescription from a doctor is not required for their purchase. Specialists, however, do not recommend giving aspirin to children without special instructions from a pediatrician, since the association of aspirin with the development of dangerous Reye syndrome has been scientifically proven.
Diagnostics
Only a doctor can accurately determine what caused inflammation in the groin or axillary lymphadenitis. Treatment, accordingly, will depend on the root cause of the pathology. For effective diagnosis, you may need:
- Studying a medical history. In addition, the doctor will ask you when and under what circumstances your lymph nodes have swollen and if you have other symptoms of malaise.
- Primary medical examination. The specialist will certainly feel the lymph nodes under the skin to assess their size, softness, warmth and texture. The place where the pathology was localized will also give a hint regarding the causes of the disease (for example, inguinal lymphadenitis in women often occurs against the background of vaginitis or inflammation of the ovaries).
- Blood tests. Assuming a particular cause of inflammation, the doctor will ask you to take specific blood tests to confirm the initial diagnosis. Often they pass an ordinary general analysis, which allows you to fairly objectively assess the patient’s health status and identify some pathologies (for example, infectious diseases or leukemia).
- Imaging studies. Often prescribed chest x-ray or computed tomography (CT) scan of the chest in order to detect potential sources of infection or tumors. So, for example, tuberculous lymphadenitis is detected.
- Biopsy. If the doctor for some reason cannot make an accurate diagnosis, he will prescribe a biopsy - a procedure in which the entire lymph node (or part of it) is removed for laboratory examination under a microscope. Diagnosis using this method may be a fine-needle aspiration biopsy (also known as aspiration diagnostic puncture). In this case, the doctor will conduct the procedure on his own during a regular medical consultation. Sometimes, however, therapists refer patients to surgeons or radiotherapy specialists to collect the biological material necessary to confirm the diagnosis of lymphadenitis.
Alternative treatment
Unfortunately, no traditional medicine will save you from such a problem as swelling and inflammation of the lymph nodes. In thematic print publications and on the Internet, you can find many recipes for infusions, decoctions and elixirs that are proposed to be used for compresses. However, experts do not recommend exposing their health to unnecessary risk, brewing herbs of dubious origin and coating the swollen lymph nodes with homemade ointments. The simplest and safest remedy for inflammation - compresses from ordinary tissue soaked in warm water and squeezed well - although it does not save you from adversity, it will really help relieve pain and reduce the sensitivity of swollen lymph nodes without any risks.
Traditional medicine
Tuberculous lymphadenitis, like some other varieties of the analyzed pathology, passes along with the accompanying infectious disease. If the swelling is caused by a viral infection, taking antibiotics is futile; in other cases, it is necessary to focus on the root cause of the development of the inflammatory process.
- Infection. If infection with microbes (bacteria) caused lymphadenitis, what antibiotics should I drink in order for the state of the lymph nodes to normalize? Be sure to ask this question to the doctor, since only the attending physician can prescribe specific drugs. If the inflammation is caused by the human immunodeficiency virus (HIV), doctors will treat the infection first.
- Immune System Disorder. In cases where the swelling of the lymph nodes is a consequence of the disease of lupus erythematosus or rheumatoid arthritis, therapy is aimed at treating the root cause of the pathology.
- Oncological diseases. Lymphadenitis in the groin, neck or armpits can be caused by the growth and spread of cancer cells. Depending on the type and stage of the cancer, treatment will include radiation therapy, chemotherapy, or surgery.