Intestinal gangrene is a necrosis of the tissues of an organ that occurs due to a violation of blood supply. Due to ischemia and lack of oxygen, cells undergo necrotic changes. This is an extremely dangerous condition that requires emergency surgery. It is already impossible to restore the function of the intestine and the dead part of the organ has to be removed. Without treatment, patients die within the first two days. But even with timely surgical intervention, the prognosis of the disease remains unfavorable.
Causes of pathology
The cause of intestinal gangrene is ischemic disease of this organ. Due to the narrowing or blockage of blood vessels, blood stops flowing into intestinal tissues. Hypoxia occurs, and then tissue necrotization.
Ischemia can be acute and chronic. In the first case, blood supply ceases instantly due to sudden blockage of blood vessels. This form of the disease is rare and very quickly leads to gangrene. Acute ischemia requires emergency medical attention.
More often, ischemia develops gradually and proceeds chronically. Such a violation of blood supply is observed in elderly patients, it is associated with atherosclerosis. In this case, at the initial stage, it is still possible to restore vascular patency with conservative methods. However, if tissue necrotization has already begun, then the only way out is surgery.
Ischemia most often occurs as a result of cardiovascular disorders. After all, the blood supply to the intestine directly depends on the work of the heart and the state of the vessels. Also, the causes of this condition can be injuries and pathologies of the digestive tract.
Forms of ischemia
What causes a violation of the blood supply to the intestines? Doctors distinguish two forms of ischemia: occlusive and non-occlusive.
Occlusive ischemia occurs due to blockage of the mesenteric veins and arteries. The following pathologies can provoke a violation of blood supply:
- atrial fibrillation;
- heart defects;
- intestinal tumors;
- diseases of the digestive tract;
- cirrhosis of the liver.
Also, the occlusive form of the disease is noted in some patients who underwent prosthetic heart valves.
Non-occlusive ischemia occurs in about half the cases. Signs of pathology develop slowly. At present, the exact reasons for this violation have not been established. It is assumed that the following diseases and conditions can provoke neocclusion ischemia:
- heart failure;
- chronic arterial hypotension;
- dehydration;
- taking medications that promote blood clotting.
It is important to remember that any form of ischemia can lead to gangrene of the intestine. Even if a violation of the blood supply develops gradually, then without treatment, sooner or later, necrotic changes in the tissues occur.
Stages of ischemia
The mortification of intestinal tissue develops in several stages. Doctors distinguish several stages of ischemia:
- Impaired blood supply. Due to a lack of nutrients in the intestinal tissues, metabolism worsens. Dystrophic changes occur in the epithelium. Because of this, the production of enzymes decreases and the digestion of food is disrupted, and peristalsis also changes. At this stage, oxygen deficiency is compensated by the flow of blood through roundabouts.
- Intestinal infarction. This stage of ischemia is considered decompensated. Blood stops flowing even along the bypass branches of blood vessels. Tissue necrosis occurs. At this stage, intestinal gangrene occurs. Photos of necrotic areas of the epithelium can be seen below.
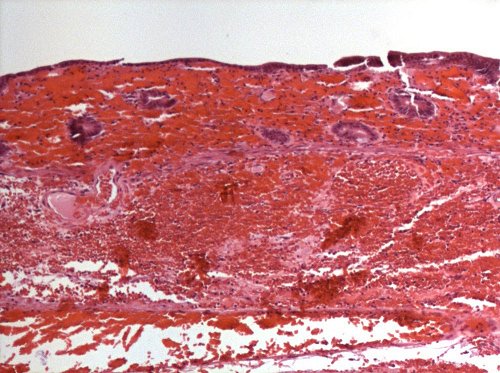
It should be noted that with decompensated ischemia, the color of the intestinal wall changes. First, due to a lack of blood supply, anemia occurs and the epithelium of the organ pales. Then blood begins to seep through the vessels. The intestinal wall turns red. Blood appears in the feces. In this case, doctors talk about hemorrhagic gangrene of the intestine, since tissue necrosis is accompanied by bleeding. As necrosis develops, the affected area becomes black.
Without surgery, necrosis very quickly leads to peritonitis. Tissue death is exacerbated by inflammation. The organ wall becomes thin and tears. The contents of the intestines go out and inflammation of the peritoneum occurs. This often causes death.
Symptoms of Ischemia
Symptoms of a blood supply disorder depend on the type of pathology. If ischemia develops suddenly and proceeds in an acute form, then the following manifestations are characteristic of it:
- There is severe pain in the abdominal cavity. It is localized in the navel or in the right upper abdomen.
- There is nausea and vomiting due to a violation of the digestion of food.
- Intestinal motility sharply increases, frequent urge to defecate and diarrhea with an admixture of blood appear.
- There is a fever.
Acute ischemia threatens the patient's life and requires immediate medical attention. About 6 hours after the first manifestations, irreversible changes occur and intestinal gangrene begins.
In chronic ischemia, symptoms develop over time and are less pronounced:
- The patient is concerned about paroxysmal abdominal pain that does not have a clear localization. They occur after eating. At the beginning of the disease, the pain is stopped by taking antispasmodics, but in advanced cases, the medications no longer help.
- Patients have a swollen abdomen; rumbling in the abdominal cavity is heard due to increased gas formation.
- The patient is often worried about nausea and vomiting.
- The bowel movement is disturbed, diarrhea alternates with constipation.
- Due to bouts of pain, a person cannot fully eat. This leads to a sharp weight loss, up to exhaustion.
Such symptoms should be the reason for immediate medical attention. Even the slow course of the disease is extremely dangerous. Chronic disturbance of blood supply can lead to an attack of acute ischemia and the rapid development of gangrene.
Signs of necrosis
Symptoms of intestinal gangrene develop about 6 hours after an attack of acute ischemia. The patient's condition is extremely serious. The following pathological manifestations are noted:
- sudden sharp weakness;
- blanching of the skin;
- unbearable abdominal pains;
- flatulence;
- vomiting
- diarrhea or delayed bowel movements;
- heart palpitations;
- weak pulse;
- a sharp drop in blood pressure;
- loss of consciousness.
Signs of pathology also depend on the location of the necrosis site. Gangrene of the small intestine is characterized by vomiting with bile and blood. As necrosis develops in the vomit, fecal impurities appear. When the colon is affected, diarrhea with blood occurs.
12-14 hours after the cessation of blood supply, peritonitis begins. The patient's pain disappears, as the nerve endings are necrotic. Gases and feces do not go away. The patient is inhibited and lethargic. In severe cases, convulsions appear, and the patient falls into a coma. This condition can be fatal within 48 hours.
Diagnostics
With gangrene, the patient needs immediate surgery and there is very little time for diagnosis. When probing the abdomen, a swollen area of the intestine with the mesentery is determined. This is a specific manifestation of necrosis.
Upon admission to the hospital, the patient is given an x-ray of the intestine. In this case, the contrast medium is not administered. If the picture shows signs of tissue destruction or peritonitis, then surgery is urgently needed.
Treatment
Surgery is the only treatment for intestinal necrosis. Dead parts of the body have to be removed. First, the surgeon restores blood supply, and then resects the affected area. After this, abdominal sanitation is done.
After surgery, the patient is prescribed a course of antibiotics and anticoagulants. Special solutions are introduced to dissolve blood clots. Do novocaine blockade to prevent intestinal cramps. It is also necessary the introduction of drugs to maintain the heart.
Drug therapy is only an additional treatment and is used after surgery. It is impossible to get rid of such a disease by conservative methods alone.
Disability
The most pronounced effects are observed in patients after surgery with gangrene of the small intestine. Is a disability group or not? This question is often of interest to patients.
During the operation, part of the intestine is removed. As a result, the length of the organ changes and its function changes. Patients have periodic abdominal pain, flatulence, diarrhea, weight loss. The condition after surgery is called short bowel syndrome (CCM). The purpose of the disability group depends on its severity:
- 3 group. It is prescribed if the manifestations of CCM are moderate or moderate, and body weight below normal is no more than 5-10 kg.
- 2 group. It is established if the patient has a severe form of CCM. Moreover, in addition to diarrhea, there are signs of vitamin deficiency and metabolic disorders, and a person loses more than 10 kg of weight.
- 1 group. It is prescribed for the most severe patients in whom CCM proceeds with complications, there are intestinal fistulas. This disability group is also established for those patients who have removed 4/5 of the small intestine.
Forecast
The outcome of the disease largely depends on how timely medical care was provided for intestinal gangrene. The prognosis of this pathology is always very serious.
Even with timely surgery, more than 50% of patients are fatal. Without surgery, mortality is 100%. Patients die from sepsis or peritonitis.
The sooner the patient is hospitalized and operated, the greater the chance of survival. If help was provided on the first day of the disease, then the prognosis is more favorable.
Prevention
How to prevent intestinal gangrene? To avoid such a dangerous disease, you need to be careful about your health. It is necessary to treat pathologies of the heart, blood vessels and gastrointestinal tract in time. If a person is often worried about abdominal pain, nausea, diarrhea and causeless weight loss, you should immediately visit a doctor. At the initial stage of ischemia, it is still possible to normalize blood circulation and avoid heavy surgery.