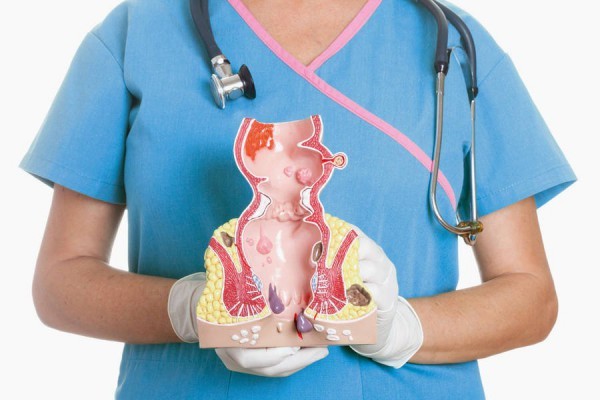
Hemorrhoids are a proctologic disease characterized by varicose hemorrhoidal veins in the rectum. Pathology can manifest itself in the form of thrombosis, expansion of veins, changes in their shape, nodes.
According to some reports, approximately 20% of the population have a history of diagnosis: hemorrhoids. And about 70% of all people at least once in their life felt a variety of symptoms of the disease, itching or discomfort in the anus.
Etiology and pathogenesis
The classification of hemorrhoids is quite extensive, but the factors that provoke the development of the disease are the same for all cases.
These can be elementary pressure surges in the veins from mechanical damage. Infectious diseases that affect the reduction of venous tone can affect the development of the disease. Some people have anatomical features that adversely affect the vascular system of the anus. Those who engage in heavy sports or are engaged in heavy physical labor often have this problem.
Pregnancy and childbirth themselves can trigger the development of hemorrhoids. If a person is in the same position for a long time or he has frequent stool disorders, then a problem can also arise. Cancerous tumors in the genitourinary system, anal opening and in the abdominal cavity can trigger the development of hemorrhoids.
Classification
To date, doctors distinguish two stages of the course of the disease:
According to the form of pathology, the disease is divided into:
Chronic form
Classification of hemorrhoids by stages:
1 | At this stage, the hemorrhoid is not falling out, but there are bloody discharge from the anus. The course of the disease is characterized by a slight change in the submucosal layer of the rectum. However, already single muscle cells are susceptible to dystrophic changes. Hemorrhoidal nodes can even swell into the lumen of the anal canal, and it is for this reason that bleeding occurs. This stage can be diagnosed only with the help of anoscopy. |
2 | This stage is already characterized by prolapse of the knot, and not necessarily with bleeding. Dystrophic processes increase, the nodes increase in size. In such a situation, an independent reduction into the anal canal often occurs. At this stage, the walls of the mucous membrane of the nodes are already seriously thinning. |
3 | At this stage, the prolapse of the node occurs more often and it constantly has to be manually adjusted. Despite serious dystrophic changes, nevertheless, the submucosal layer of the rectum retains its elasticity, therefore, it can perform its functions almost completely. |
4 | At this stage, there is a constant loss of hemorrhoidal nodes. But not only the nodes, but also the mucous membrane of the rectum, already fall out, therefore, it will not be possible to produce a self-reduction. As in other stages, everything happens with or without bleeding. This stage is characterized by almost complete replacement of elastic cells by connective tissue, multiple ruptures are observed on the ligamentous apparatus. |
Acute form
This form is actually a complication of the chronic form. Classification of acute hemorrhoids consists of three stages:
- Thrombosis without an inflammatory process on the internal and external hemorrhoids.
- Thrombosis, but with an already inflammatory process.
- At the third stage, the inflammatory process on the subcutaneous tissue already begins, swelling on the perianal skin may appear, and mucosal necrosis may develop.
Classification of hemorrhoids by degrees reflects the pathogenesis of pathology and gives doctors the opportunity to objectively evaluate the indications and adequately choose the course of treatment.
Most often, the pathology proceeds against the background of a change in the chronic stage to an acute inflammatory process. Acute provocateurs include:
- increased constipation;
- inflammation of the perineum, anal canal, or rectum.
Such processes lead to the fact that thrombosis increases, and the inflammatory process passes to the surrounding tissue.
Diagnostics
The simplest examination technique is on a gynecological chair, when the patient presses his legs to the stomach as much as possible, or the examination can be carried out in the knee-elbow position. The doctor also evaluates which clinic, classification of hemorrhoids. Upon examination, it evaluates the condition of the anus, its gaping, determines whether there are deformations or other changes, the possibility of self-adjustment of the node.
A probe is already used to determine the presence or absence of an anal fissure.
The finger method allows you to determine the tonic state of the sphincters, volitional contractions. Also, this method allows you to identify scars, polyps and mucosal defects. Although the technique does not allow to determine with full confidence the size and location of the nodes.
Anoscopy is the most effective way to determine the presence of a disease at an early stage. This is an instrumental technique that is fairly well tolerated by patients and allows you to assess the condition of the anal canal at a distance of 8-12 centimeters.
Also, to clarify the diagnosis and classification of hemorrhoids, sigmoidoscopy or colonoscopy is performed. Despite the fact that these examinations cannot completely replace the examination by a proctologist, they make it possible to identify concomitant pathologies. Indeed, according to statistics, every third patient with diagnosed hemorrhoids reveals other diseases, both in the anus and in the colon or rectum, which, in fact, lead to bleeding.
Often against the background of hemorrhoids, an anal fissure is revealed, which occurs due to chronic microtrauma of the mucous membrane.
Particular attention in the diagnosis is given to patients who often have bleeding, because they can talk not only about the presence of hemorrhoids, but also about the development of cancer in the rectum or colon.
Treatment of the 1st stage of the disease
Depending on the classification of hemorrhoids, a treatment method is selected. In the first stage of the chronic form, they resort to conservative treatment, less often to sclerotherapy or infrared photocoagulation.
Conservative or drug therapy is aimed at stopping the unpleasant symptoms that accompany the disease, and preventing possible complications. To date, a fairly large arsenal of medicines, the effect of which has been well studied. First of all, rectal suppositories are used.
There is even a classification of suppositories for hemorrhoids:
- With analgesic effect. In such preparations, novocaine or anestezin is present. The main side effect of such suppositories is a strong increase in blood pressure in the patient.
- Hemostatic. The action of such suppositories is aimed at increasing blood coagulation. The composition of the funds may include: vicasol, calcium chloride, dicinone.
- Suppositories that reduce the inflammatory process. Such agents also have a bactericidal effect. The composition of medicines usually contains sea buckthorn oil, propolis, St. John's wort and other natural ingredients that accelerate the healing process.
Today, the most popular candles are called Relief. In addition to suppositories, gels and ointments can be used, which also contribute to the removal of the inflammatory process, for example: "Aurobin", ointment "Heptrombin G". Pregnant women are recommended to use natural-based preparations, for example, Natalsid.
Depending on the classification of hemorrhoids and the degree of pain, tableted forms of drugs based on analgesics, as well as venotropic and laxatives, can be prescribed.
Sclerotherapy may be recommended at this stage. This operation is completely uncomplicated and lasts only a few minutes, painless. Patients who have passed this stage will forever lose their discomfort in the anus.
Stage 2 Treatment
At this stage, methods are also used, as in the first stage of the disease.
The infrared coagulation technique allows the infrared light flux to penetrate into the tissue of the node and coagulate the tissue. This procedure is recommended in the presence of bleeding. Depending on the classification of hemorrhoids and the severity of symptoms, from 1 to 6 coagulations can be performed. However, this technique can lead to a number of complications: pain, necrosis of the mucosa, thrombosis of the node.
Ligation with latex rings is read by a radical measure, but residually effective. This procedure is indicated only in the 2nd or 3rd stage of the disease. There are two ways of carrying out the procedure, but in both cases, elastic latex rings are used, which compress the tissues of the hemorrhoidal node for 12-14 days, with a phased intersection of the legs. This technique allows you to avoid hemorrhoidectomy in 80% of cases.
At this stage of the disease, combined treatment methods can be used.
Stage 3 treatment
If according to the classification of hemorrhoids it is already possible to talk about the 3rd stage, then in addition to ligation with latex rings, transanal resection of the mucosa according to the Longo method can be proposed. The essence of the technique is to remove a small area of the rectal mucosa. The wound is then sutured with titanium staples. And most importantly, the nodes themselves are not removed, but contracted, that is, the volume of blood flow decreases. Over time, the blood supply to the nodes becomes not so intense, and the nodes are tightened by connective tissue.
Stage 4 Treatment
If, according to the classification of chronic hemorrhoids, the 4th stage has already been determined, the patient's ability to work decreases sharply, with defecation the hemorrhoidal node regularly falls out, then there is only one way out - hemorrhoidectomy, that is, surgical intervention. This method is also used in the case of diagnosing an external hemorrhoid.
Drug prophylaxis
Despite the little knowledge of the importance of drug therapy in the prevention of hemorrhoids, the doctor nevertheless determines its necessity individually when examining each patient. There is a risk group that includes people with a sedentary lifestyle, with a lot of overweight, women during pregnancy, or people who consume large amounts of alcohol.