Different people have different ability of insulin to stimulate glucose uptake. It is important to know that a person may have normal sensitivity to one or more effects of this compound and at the same time - absolute resistance to others. Next, we examine the concept of "insulin resistance": what it is, how it manifests itself.
General information
Before analyzing the concept of "insulin resistance", what it is and what signs it has, it should be said that this disorder is common enough. More than 50% of people with hypertension suffer from this pathology. Most often, insulin resistance (what it is, will be described below) is found in the elderly. But in some cases, it is detected in childhood. The insulin resistance syndrome often remains unrecognized before metabolic disturbances begin to appear. The risk group includes people with dyslipidemia or impaired glucose tolerance, obesity, hypertension.
Insulin resistance
What it is? What features does the violation have? The metabolic syndrome of insulin resistance is an incorrect response of the body to the action of one of the compounds. The concept is applicable to various biological effects. This, in particular, relates to the effect of insulin on protein and lipid metabolism, gene expression, and vascular endothelial function. The impaired response leads to an increase in the concentration of the compound in the blood relative to the amount of glucose needed for the available volume. Insulin resistance syndrome is a combined disorder. It involves a change in glucose tolerance, type 2 diabetes, dyslipidemia, and obesity. "Syndrome X" also implies resistance to glucose uptake (insulin-dependent).
Development mechanism
To date, specialists have not been able to fully study it. Disorders that lead to the development of insulin resistance can occur at the following levels:
- Receptor. In this case, the condition is manifested by affinity or a decrease in the number of receptors.
- At the level of glucose transport. In this case, a decrease in the number of GLUT4 molecules is detected.
- Prereceptor. In this case, they speak of abnormal insulin.
- Postreceptor. In this case, there is a violation of phospholation and a violation of signal transmission.
Anomalies of insulin molecules are quite rare and do not have clinical significance. Receptor density may be reduced in patients due to negative feedback. It is caused by hyperinsulinemia. Often patients have a moderate decrease in the number of receptors. In this case, the feedback level is not considered a criterion by which it is determined to what extent insulin resistance is. The causes of the disorder are reduced by specialists to postreceptor disturbances in signal transmission. Provoking factors, in particular, include:
- Smoking.
- The increase in the content of TNF-alpha.
- Decreased physical activity.
- Increased concentration of non-esterified fatty acids.
- Age.
These are the main factors that more often than others can provoke insulin resistance. Treatment includes the use of:
- Diuretics of the thiazide group.
- Beta-adrenoreceptor blockers.
- Nicotinic acid.
- Corticosteroids.
Increased insulin resistance
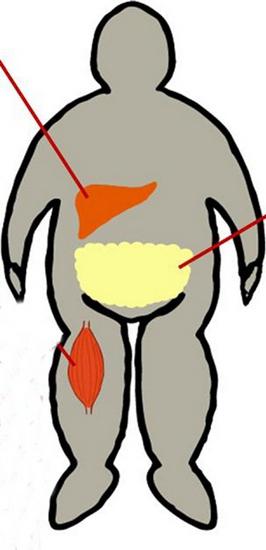
The effect on glucose metabolism occurs in adipose tissue, muscle and liver. Skeletal muscle metabolizes approximately 80% of this compound. Muscles in this case act as an important source of insulin resistance. Capture of glucose into the cells is carried out by means of a special transport protein GLUT4. Upon activation of the insulin receptor, a series of phospholation reactions is triggered. They ultimately lead to translocation of GLUT4 into the cell membrane from the cytosol. So glucose gets the opportunity to enter the cell. Insulin resistance (the norm will be indicated below) is caused by a decrease in the degree of translocation of GLUT4. At the same time, there is a decrease in the use and uptake of glucose by cells. Along with this, in addition to facilitating glucose uptake in peripheral tissues, production of glucose by the liver is suppressed with hyperinsulinemia. With type 2 diabetes, it resumes.
Obesity
It is combined with insulin resistance quite often. If the patient exceeds the weight by 35-40%, the sensitivity decreases by 40%. The adipose tissue located in the anterior abdominal wall has a higher metabolic activity than the one located below. In the course of medical observations, it was found that an increased release of fatty acids from the abdominal fibers into the portal blood stream provokes the production of triglycerides by the liver.
Clinical signs
Insulin resistance, the symptoms of which are mainly associated with metabolic disorders, can be suspected in patients with abdominal obesity, gestational diabetes, a family history of type 2 diabetes, dyslipidemia, and hypertension. At risk are women with PCOS (polycystic ovary). Due to the fact that obesity is a marker of insulin resistance, it is necessary to assess the nature of the distribution of fatty tissue. Its location can be gynecoid - in the lower part of the body, or android type - in the front wall of the peritoneum. Accumulation in the upper half of the body is characterized by a more significant prognostic factor for insulin resistance, altered glucose tolerance and diabetes than obesity in the lower parts. To identify the amount of fatty abdominal tissue, you can use the following method: determine the ratio of waist, hips and BMI. At rates of 0.8 for women and 0.1 for men and a BMI of more than 27, abdominal obesity and insulin resistance are diagnosed. Symptoms of pathology manifest themselves externally. In particular, wrinkled, rough hyperpigmented areas are noted on the skin. Most often they appear in the armpits, on the elbows, under the mammary glands. The analysis for insulin resistance is a calculation according to the formula. HOMA-IR is calculated as follows: fasting insulin (μU / ml) x fasting glucose (mmol / l). The result is divided by 22.5. The result is an insulin resistance index. The norm is <2.77. With a deviation in the direction of increase, a tissue sensitivity disorder can be diagnosed.
Disorders of other systems: vascular atherosclerosis
Today, there is no single explanation for the mechanism of the influence of insulin resistance on damage to the cardiovascular system. Direct effects on atherogenesis may be noted. It is caused by the ability of insulin to stimulate lipid synthesis and proliferation of smooth muscle components in the vessel wall. At the same time, atherosclerosis can be caused by concomitant metabolic disorders. For example, it can be hypertension, dyslipidemia, changes in glucose tolerance. In the pathogenesis of the disease, the impaired function of the vascular endothelium is of particular importance. His tasks include maintaining the tone of the blood channels through the secretion of mediators of vasodilation and vasoconstriction. In the normal state, insulin provokes relaxation of the smooth muscle fibers of the vascular wall during the release of nitric oxide (2). At the same time, its ability to enhance endothelium-dependent vasodilation significantly changes in patients with obesity. The same applies to patients with insulin resistance. With the development of the inability of the coronary arteries to respond to normal stimuli and expand, we can talk about the first stage of microcirculatory disorders - microangiopathy. This pathological condition is observed in most patients with diabetes (diabetes mellitus).

Insulin resistance can provoke atherosclerosis through disturbances in the process of fibrinolysis. IAP-1 (plasminogen activator inhibitor) is in high concentration in patients with diabetes and obesity without diabetes. The synthesis of IAP-1 is stimulated by proinsulin and insulin. The level of fibrinogen and other procoagulant factors is also increased.
Altered glucose tolerance and type 2 diabetes
Insulin resistance is a precursor to the clinical manifestation of diabetes. Beta cells in the pancreas are responsible for the decrease in glucose concentration. The decrease in concentration is carried out by increasing the production of insulin, which, in turn, leads to relative hyperinsulinemia. Euglycemia can persist in patients for as long as beta cells will be able to maintain a fairly high plasma insulin level in order to overcome resistance. Ultimately, this ability is lost, and the concentration of glucose increases significantly. The key factor that is responsible for fasting hyperglycemia in the presence of T2DM is hepatic insulin resistance. A healthy response is to lower glucose production. With insulin resistance, this reaction is lost. As a result, the liver continues to produce excessive glucose, which leads to fasting hyperglycemia. With the loss of the ability of beta cells to provide insulin hypersecretion, there is a transition from insulin resistance with hyperinsulinemia to altered glucose tolerance. Subsequently, the condition is transformed into clinical diabetes and hyperglycemia.
Hypertension
There are several mechanisms that determine its development against the background of insulin resistance. As observations show, the weakening of vasodilation and activation of vasoconstriction can contribute to increased vascular resistance. Insulin stimulates the nervous (sympathetic) system. This leads to an increase in plasma concentrations of norepinephrine. Patients with insulin resistance have an increased response to angiotensin. In addition, vasodilation mechanisms may be impaired. In a normal state, the administration of insulin provokes relaxation of the muscular vascular wall. In this case, vasodilation is mediated by the release / production of nitric oxide from the endothelium. In patients with insulin resistance, endothelial function is impaired. This leads to a decrease in vasodilation by 40-50%.
Dyslipidemia
With insulin resistance, the normal suppression of the release of fatty free acids after eating from adipose tissue is disrupted. Increased concentration forms a substrate for enhanced synthesis of triglycerides. This is an important step in the production of VLDL. With hyperinsulinemia, the activity of an important enzyme, lipoprotein lipase, decreases. Among the qualitative changes in the LDL spectrum against type 2 diabetes and insulin resistance, an increased degree of oxidation of LDL particles should be noted. More susceptible to this process are glycated apolipoproteins.
Therapeutic measures
Increasing insulin sensitivity can be achieved in several ways. Of particular importance is weight loss and physical activity. Diet is also important for people who are diagnosed with insulin resistance. Diet helps to stabilize for several days. Sensitivity will be further enhanced by weight loss. For people who have established insulin resistance, treatment consists of several stages. Stabilization of diet and physical activity is considered the first stage of therapy. For people with insulin resistance, the diet should be low in calories. A moderate decrease in body weight (by 5-10 kilograms) often contributes to improved control over glucose levels. Calories are 80-90% distributed between carbohydrates and fats, 10-20% are proteins.
Medications
Means "Metamorphine" refers to medicines of the biguanide group. The drug helps to increase peripheral and liver sensitivity to insulin. In this case, the agent does not affect its secretion. In the absence of insulin, the Metamorphine preparation is ineffective. The drug "Troglitazone" is the first medication of the thiazolidinedione group, which is approved for use in the United States. The drug enhances glucose transport. This is probably due to activation of the PPAR gamma receptor. And due to this, the expression of GLUT4 is enhanced, which, in turn, leads to an increase in insulin-induced glucose uptake. For patients who have insulin resistance, treatment can be prescribed and combined. The above funds can be used in combination with sulfonylurea, and sometimes with each other to obtain a synergistic effect on plasma glucose and other disorders. The drug "Metamorphine" in combination with sulfonylurea enhances secretion and sensitivity to insulin. At the same time, glucose levels decrease after eating and on an empty stomach. In patients who were prescribed combination treatment, manifestations of hypoglycemia were more often noted.