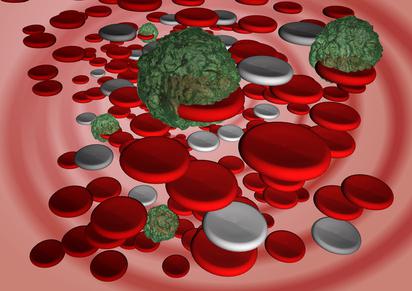
The state of the body's predisposition to the development of vascular thrombosis, which can recur and have different localization, is called thrombophilia. The disease can be either genetic or acquired. The cause of the pathology most often is increased blood clotting. Clinically, the disease can manifest itself in many thromboses of different localization. Thrombophilia is quite common among the population and occurs in various forms. The disease requires treatment with medical or surgical methods.
Thrombophilia: what is it?
Pathology refers to diseases of the blood system, manifests itself in a tendency to form blood clots and impaired hemostasis. Multiple recurrent thromboses in thrombophilia can occur as a result of injuries, surgery, physical strain, or during pregnancy. The condition is dangerous in that it can lead to complications such as pulmonary embolism, stroke, myocardial infarction, deep vein thrombosis. Often, neglected forms are fatal.
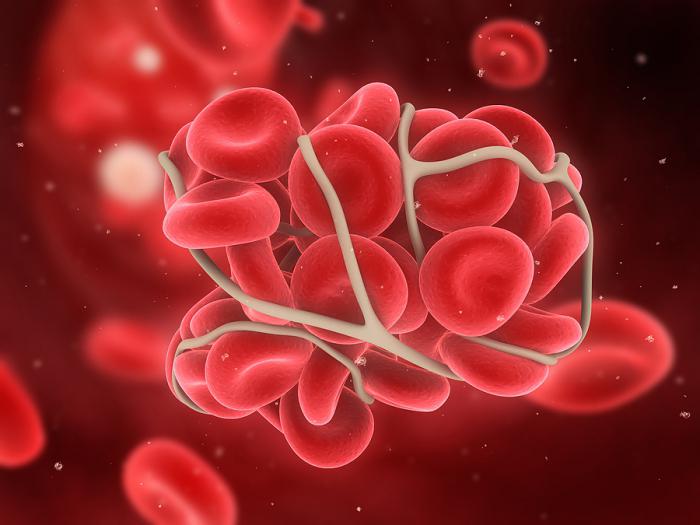
Several areas of medicine are involved in the research, diagnosis, and treatment of thrombophilia. Hematology studies violations of blood properties, phlebology - methods for diagnosing and treating venous thrombosis, vascular surgeons are involved in the removal of blood clots. The formation of a blood clot leads to a violation of normal blood flow, which is accompanied by the development of dangerous conditions that are difficult to treat. In order to prevent a problem in time, you need to periodically take a blood coagulation test. The norm in women, for example, for venous blood is 5-10 minutes.
Development reasons
There are several factors that cause the development of pathology. Almost everyone can experience a disease like thrombophilia. What is this dangerous condition, many patients sometimes do not even suspect and seek help quite late. There is a list of reasons that may contribute to the development of pathology.
Hereditary (or genetic) thrombophilia results from a genetic predisposition to the disease. Previously transferred blood diseases (thrombocytosis, erythremia, antiphospholipid syndrome) can also be the cause of its development. Dangerous factors include atherosclerosis, malignant neoplasms, atrial fibrillation, varicose veins, autoimmune diseases. The likelihood of thrombophilia increases after a stroke or heart attack. Patients who are obese, lead a sedentary lifestyle, take hormonal contraceptives, eat improperly, and have suffered a serious injury or surgery in the past are at risk. At an early age, the disease is rare, it most often develops in older people. To prevent the disease or not start the condition, it is recommended that you undergo a thrombophilia test from time to time.
Clinical picture
Clinical manifestations of the pathology are characterized by a smooth increase and duration of the course, so patients do not immediately notice changes in their health status and do not show any complaints. Laboratory indicators can diagnose thrombophilia, and a detailed clinical picture in some cases appears only a few years later. Vivid symptoms are observed when a blood clot has already formed. The degree of obstruction of the lumen of the vessel and the localization of the thrombus affect the severity of symptoms.
Arterial thrombosis, the causes of which are blood clots in the lumen of the vessels of the arterial bed, is accompanied by the formation of blood clots in the lumen of the vessels of the placenta, intrauterine death of the fetus, repeated miscarriages, attacks of acute coronary insufficiency, ischemic stroke.
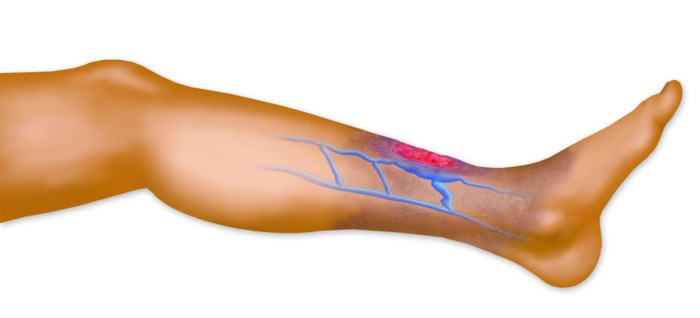
With venous thrombosis of the lower extremities, clinical symptoms appear in the form of trophic changes in the skin, severe swelling of the lower extremities, the appearance of pain, a feeling of heaviness in the lower extremities.
Mesenteric intestinal thrombosis occurs when a thrombus is localized in mesenteric vessels and is accompanied by such symptoms: loose stools, vomiting, nausea, acute dagger pain.
With thrombosis of the veins of the liver, hydrothorax (Budd-Chiari syndrome), ascites, edema of the anterior abdominal wall and lower extremities, indomitable vomiting and intense pain in the epigastric region develop.
Hematogenous thrombophilia
Thromboses affect the state of the vascular wall, damaging it and decreasing resistance, contribute to slowing blood flow and the development of other hemodynamic disorders that are associated with changes in viscosity and coagulation. Thrombophilic conditions in many cases are associated with the presence of vascular diseases, such as atherosclerosis, damage to vascular intima, vasculitis of toxicogenic, immune or infectious origin. Multiple recurrent thromboembolism may be due to changes in the properties of the blood itself, which gives the right to talk about a disease called "hematogenous thrombophilia." The development of pathology is associated with the tendency of the body to develop thrombosis due to abnormalities in the coagulation systems, a violation of the hemostatic potential of the blood.

Hematogenous thrombophilia can be congenital or acquired by origin. The main mechanism distinguishes diseases that are caused by: conjugated thrombogenic changes, platelet dysfunction, fibrinolysis disorders, inhibition, abnormalities or deficiency of blood coagulation, lack of basic physiological anticoagulants. In addition, iatrogenic thrombophilia developing as a result of drug treatment or medical interventions is also isolated.
Hereditary thrombophilia
The congenital or hereditary nature of thrombosis can be determined on the basis of the following clinical manifestations: thrombosis at an early age, cases of pulmonary artery thrombosis, mesentery, lower extremities in a family history, the first episode of recurrent venous thrombosis before 30 years of age, thrombosis during early pregnancy, thrombotic complications. Hereditary or genetic thrombophilia is determined after a comprehensive diagnosis of patients who are at risk of developing thrombophilic complications.
The congenital form of the disease can have a different nature. When diagnosing a disease, genetic markers of thrombophilia are taken into account. The first factor that contributes to the development of pathology is a genetic predisposition. In this case, the disease may not appear in the absence of conditions that trigger the mechanisms of its development. The second is gene mutation during embryonic development. Recently, the concentration of factors pushing for gene mutations has been noticeably increasing. Among them are those that arise from human activities: radiation, the use of food additives, medicines, environmental pollution (household chemicals, various fuels, pesticides), technological disasters. It is impossible to predict under what conditions a gene can give in to changes, therefore, mutagenesis is considered a random process that occurs on its own and has the ability to change hereditary properties.

Hereditary thrombophilia can also be caused by a structural or genomic mutation of chromosomes inherited from previous generations. Here the state of the gene of the disease matters: recessive or dominant. In the second case, the pathology will manifest itself under any conditions.
Acquired Thrombophilia
Not only hereditary, but also acquired origin can have this disease. The patient may be diagnosed with antiphospholipid syndrome (APS). That is how in most cases acquired thrombophilia manifests itself. What is it, what are the mechanisms of its development and how to deal with it?
Antiphospholipid syndrome is a complex of symptoms that combines laboratory data and clinical signs. The disease is accompanied by neurological disorders, immune thrombocytopenia, fetal loss syndrome, venous and arterial thrombosis. The forms of APS are distinguished: primary, secondary and catastrophic; serological options: seronegative and seropositive. The syndrome occurs against the background of tumor, infectious, allergic or autoimmune diseases or due to drug intolerance.
The development of AFS can be associated with pathological conditions such as malignant neoplasms (cancer, lymphoproliferative diseases, leukemia), infections (mycoplasmosis, HIV, syphilis), asymptomatic circulation of AFA, chronic kidney failure, diseases of peripheral arteries and heart valves, liver diseases, connective tissue diseases and autoimmune diseases (Crohn's disease, systemic vasculitis, SLE).
Thrombophilia during pregnancy
During pregnancy, genetic or hereditary thrombophilia often manifests itself for the first time. This is primarily due to the appearance of a third, placental circle of circulation, which puts an additional burden on the circulatory system. The formation of blood clots also contributes to a number of features of the placental circle. There are no capillaries in the placenta, the mother’s blood from the arteries enters it, then, flowing through the villi of the chorion, it enters the umbilical cord.
The body of a pregnant woman is characterized by increased blood coagulation, which ensures a decrease in blood loss during childbirth or in the event of complications such as a miscarriage or placental abruption. It helps to increase the risk of blood clots, and in fact it is a danger in them. If they are localized in the vessels that lead to the placenta, nutrients cease to flow into the fetus, and hypoxia occurs. Depending on the level of vascular occlusion and the number of blood clots, severe complications can follow: premature birth, miscarriage, miscarriage, malformations or death of the fetus, placental insufficiency, placental abruption. They appear, as a rule, after 10 weeks. At earlier stages, thrombophilia during pregnancy is very rare. If the disease develops after 30 weeks, then it ends in many cases with placental abruption, placental insufficiency or severe forms of gestosis. During the examination, the doctor should pay attention to blood coagulation, the norm in women "in position" which is slightly different from the generally accepted one.
Diagnostics
The clinical manifestations of thrombosis are confirmed in the clinic using laboratory (cytological, biochemical, genetic, coagulological) and instrumental methods. The appearance and condition of the body can determine the suspicion of venous thrombosis (edema). Both venous and arterial are accompanied by constant pressing pains and a feeling of fullness. Sometimes in the area of localization, skin temperature (venous) rises. With arterial thrombosis near the site of thrombus formation, a decrease in temperature, cyanosis (cyanosis), and sharp pain are observed. The listed symptoms are the first markers of thrombophilia, which are the most important reason to visit a specialist.
Directly in the hospital conduct more thorough studies of the patient's condition. It is necessary to take an analysis for thrombophilia, make an ultrasound of the vessels (determines the nature, size and location of the thrombus), conduct contrast arteriography and venography, which allows you to localize and study the anatomy of thrombotic processes. In addition, X-ray, radioisotope methods, genetic analysis of polymorphisms, and determination of homocysteine concentration are used.
Treatment
The question of overcoming the disease arises in those who are faced with a diagnosis of thrombophilia. What is it and how to deal with it in order to avoid serious consequences? Treatment of pathology should be comprehensive and be carried out with the participation of doctors of different specializations: vascular surgeon, phlebologist, hematologist. At the first stage, it is necessary to study the etiopathogenetic mechanisms of the development of the disease. Positive results from treatment should be expected only after eliminating the root cause. An important element of therapy is a diet, which consists in the exclusion of foods with high cholesterol, limiting fatty and fried foods. It is recommended to include dried fruits, vegetables and fruits, fresh herbs in the diet.
Drug treatment consists in the appointment of antiplatelet agents, which is supplemented by the use of anticoagulant therapy, curative bloodletting, hemodelution. In some cases, transfusion of freshly frozen plasma in combination with heparinization should be performed. Substitution therapy is prescribed in the hereditary form, which is caused by a deficiency of antithrombin III.
Mild thrombophilia (a blood test will help determine the shape) is treated using lyophilized plasma (intravenous) or dry donor plasma. In severe forms, fibrinolytic drugs are used, which are administered at the level of the clogged vessel using a catheter. With a diagnosis of thrombophilia, treatment should be individually selected and comprehensive, which will ensure a quick and effective recovery.
Prevention
In order not to encounter this serious disease or its complications, it is necessary to periodically carry out preventive measures to prevent it. Patients with thrombophilia are advised to carry out plasma transfusions in low doses and subcutaneous administration of the heparin drug. For prevention, the patient should be prescribed medications that strengthen the vascular wall (Trental intravenously, Papaverine orally).
For the prevention and treatment of thrombophilia, it is recommended to use folk remedies, for example, medicinal plants. So, cranberry tea or grape juice will help reduce platelet activity. Blood can be destroyed with the help of tincture from the seeds of Japanese sophora. In addition, it is advisable to draw up a proper diet, often walk in the fresh air and abandon bad habits.