Transient ischemic attack (TIA) is manifested by an acute violation of cerebral circulation, all the consequences of which are restored within a day after their formation. Such manifestations are temporary and pass on their own, so they are called transient. Many patients with such attacks do not go to the doctor. Although statistics show that more than half of patients with stroke suffered prior to this TIA. ICD-10 transient ischemic attack has a common code G45. A more detailed encryption indicates the location of violations. For example, a code with temporary memory loss is indicated by G45.4. Most often, this disease affects older people.
What is transient ischemic attack?
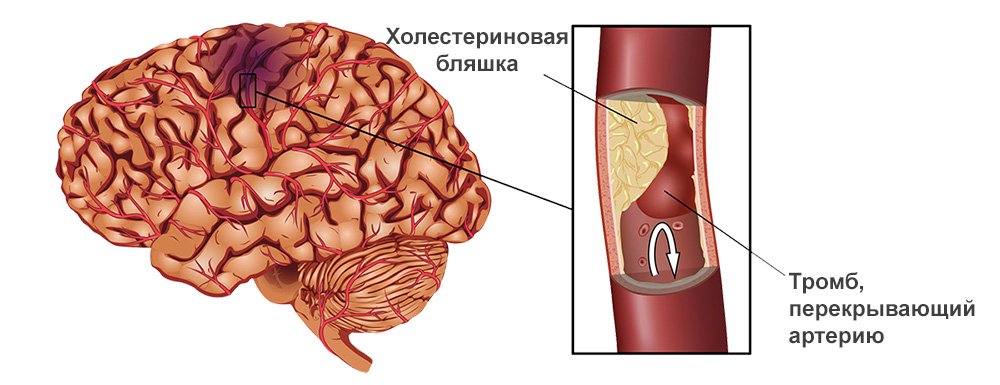
This is a temporary circulatory disorder in the brain. Otherwise, it is called a microstroke. TIA is a critical condition that portends an impending stroke. Nevertheless, in no more than 24 hours, it passes without the development of a heart attack center. A transient ischemic attack is formed when one of the vessels supplying the brain is blocked. The blood flow through the vessel is blocked by the resulting atherosclerotic plaque or thrombus.
Due to a lack of blood in some parts of the brain, oxygen starvation begins, and their functioning is disturbed. In some cases, the disease occurs due to hemorrhage, but in this case, blood circulation is quickly restored. The disease is insidious in that it is not taken seriously, its manifestation is considered overwork or a consequence of stress. Sometimes symptoms occur in a dream, and the patient simply does not suspect that he had a transient ischemic attack, since there were no consequences. Therefore, neurologists are advised to undergo an examination once a year for the purpose of prevention.
TIA classification
According to the severity of the disease, the following degrees are distinguished:
- Mild - symptoms appear for about ten minutes, and then everything recovers. With this course, patients do not attach importance to the disease and do not consult a doctor, but after some time the attacks are repeated.
- Medium - signs can be observed up to several hours, but no consequences occur.
- Severe - symptoms remain during the day.
At the location of the thrombus, in connection with the international classification, transient ischemic attack has one of the following options for the course of the disease:
- carotid artery syndrome;
- global short-term amnesia;
- unspecified forms;
- multiple bilateral symptoms of cerebral arteries;
- arterial vertebrobasilar system syndrome;
- transient blindness.
The causes of the disease
For the development of the disease, there are many different prerequisites that have a negative effect on the state of the vessels of the brain and blood coagulation. The following factors are considered to be the main factors contributing to the development of transient ischemic attack:
- Osteochondrosis of the cervical spine.
- High blood pressure.
- Thromboembolism resulting from heart diseases: arrhythmias, myocardial infarction, valve malformations, endocarditis, chronic heart failure.
- Progressive atherosclerotic vascular changes. As a result, cholesterol plaques are formed, which are distributed with blood through the vessels and can block them, slowing down the blood flow.
- Diabetes.
- Failures in the metabolic processes.
- Atrial fibrillation.
- Abnormal tortuosity of cerebral vessels.
- Autoimmune and inflammatory diseases of the blood vessels.
- Antiphospholipid syndrome.
- Angiopathy, which is manifested by dystonia, temporary reversible spasms and paresis of blood vessels.
- Bleeding and coagulopathy (bleeding disorder). These phenomena also lead to blood clots and blockage of blood vessels.
- Migraine.
Risk factors and causes of transient ischemic attack include the following:
- artificial heart valves;
- alcoholism: poisoning of the body or its systematic use, even in small doses;
- tobacco abuse;
- low physical activity.
The more people have provocative factors, the higher the risk of TIA. In children with severe heart ailments and endocrine diseases, symptoms of transient ischemic attack appear.
TIA in children
Basically, the disease is diagnosed in people of an older age category, this is due to the natural aging of the body. What causes TIA in children and adolescents? Among the important factors in the development of the disease is:
- atherosclerosis of the arteries of the neck and head;
- various deviations of the vascular bed;
- the formation of blood clots in the cavities of the heart and valves, associated with a violation of blood coagulation, uncoordinated contraction of the heart muscle and infections.
To determine the exact cause of the transient ischemic attack in children, a complete examination is necessary. First of all, parents should show their child a neurologist who:
- conduct a conversation and find out all the details of the occurrence of the disease, tolerance of physical exertion, learns a family history;
- to determine the patency of the vessels of the brain will appoint a study using CT or MRI;
- EEG (electroencephalogram) will help to eliminate epilepsy.
The next doctor is a pediatrician. Most likely, a comprehensive analysis of blood coagulation indicators will be required, with which it is possible to exclude or confirm congenital diseases associated with it. The process of blood clots also develops as a result of teenage use of contraceptives, frequent visits to the solarium, the use of dietary supplements, drugs or alcohol. The next important reason is a tumor, which may result in thrombosis. For its detection, CT and MRI data are used.
It is necessary to conduct a blood test for the amino acid homocysteine. In people with a deficiency of vitamin B6 and B12, its level rises, and this contributes to the development of atherosclerosis and provokes thrombosis.
The hereditary predisposition of the child to high blood cholesterol also contributes to early atherosclerosis. To confirm this, a blood test for lipoprotein A.
It remains to visit a cardiologist who listens to heart sounds and tones. To determine the pathologies, an electrocardiogram, an ultrasound of the heart and blood vessels of the neck are necessary. Your doctor will look for birth defects that can cause abnormal blood flow and blood clots.
Examinations will take a lot of time, but they are necessary to identify the reasons in order to undergo timely treatment of transient ischemic attack and to prevent further development of the disease.
Blood supply to the brain
Symptoms of the disease depend on in which area of the brain the damaged vessels are located. There are two vascular pools:
- Carotid, where the carotid arteries are located . They affect the blood supply to the cerebral hemispheres, which are responsible for sensitivity, motor activity and higher nervous activity.
- Vertebral-basilar, contain vertebral and basilar arteries supplying the brain stem. This part of the brain is responsible for vital functions: vision, blood circulation, memory, respiration.
Symptoms of transient ischemic attack in case of circulatory disorders in the carotid pool
Manifestations of the disease:
- Disturbed motor ability in the extremities. Often this happens on one side: the left arm and leg, or in only one limb. In some cases, paralysis in the whole body is possible.
- There is no sensitivity in half of the body (left or right), or in both at the same time.
- Paralysis of half of the face. With a smile, an asymmetric uplift of the upper lip is observed.
- Speech is upset: there is a fuzziness of the spoken words, there is no ability to understand what has been heard, and your own speech may be incoherent and incomprehensible in meaning, an inability to pronounce the words appears, or there is a complete lack of speech.
- Visual impairment: both or one eyeball stop moving, partial or complete blindness occurs.
- Intellectual abilities disappear: the patient cannot say where he is, to determine the time.
- Failure in higher nervous activity is manifested by the inability to write and read.
Symptoms caused by impaired circulation in the vertebral-basilar pool
In this case, signs of transient ischemic attack are manifested:
- gait instability - rocking from side to side;
- constant dizziness - it seems that all objects are spinning;
- headaches in the occipital part;
- sweeping and inaccurate movements;
- trembling in the limbs;
- limited movement of the eyeballs of one or both eyes;
- tinnitus;
- loss of sensation in one half of the body or throughout the body;
- delayed and irregular breathing;
- impaired ability to move limbs;
- unexpected loss of consciousness.
Diagnosis of the disease
With the rapid course of TIA, the symptoms of the disease will most likely disappear before the arrival of an ambulance or visiting a doctor, therefore, when conducting a diagnosis of transient ischemic attack, the following examinations are required:
- To analyze the patient’s complaints and to collect a medical history: find out how much time has passed after the first symptoms, whether vision, gait, sensitivity were impaired, whether heart or vascular diseases were diagnosed before.
- Conduct a visual examination of the patient for the presence of loss of vision, sensitivity, movement of the limbs.
- Blood test for the level of coagulability.
- Urine analysis to check liver and kidney function.
- CT scan - to determine vascular obstruction.
- ECG - detects signs of heart rhythm failure.
- Ultrasound of the heart - performed to detect blood clots.
- Ultrasound of vessels located at the level of the neck and feeding the brain.
- TCD - the blood flow of the arteries located in the skull is assessed.
- MRI - the patency of the arteries inside the skull is visible.
- If necessary, consult a therapist.
Based on the collected history, analysis results and data obtained during the examination, the patient is given an accurate diagnosis, and the doctor prescribes the appropriate course of treatment.
TIA treatment
Clinical recommendations for transient ischemic attack are aimed at therapy, which should focus on eliminating the causes of the disease and preventing relapse. For a speedy recovery, treatment begins immediately after the patient seeks medical help. He is hospitalized in the Department of Neurology. For therapy, the following groups of drugs are used:
- Lowering blood pressure. They begin to be used on the second day after the disease, otherwise there will be a decrease in the blood supply to the brain.
- Anticoagulants - reduce blood coagulation activity, prevent blood clots from forming.
- Statins - used to treat transient ischemic attack. They help prevent atherosclerosis and lower blood cholesterol.
- Neuroprotectors - improve brain nutrition.
- Antiarrhythmic - restore heart rate.
- Coronarolytics - relieve spasm of blood vessels.
- Improving cerebral circulation.
- Nootropics - to maintain the work of neurons.
Complications and consequences
With a quick response to symptoms and timely treatment, a person returns to normal life after a short period of time. The consequence of a transient ischemic attack, not treated in a timely manner, is an ischemic stroke, which develops in half of all people who have had the disease. As a result, persistent neurological defects are formed:
- paralysis - impaired limb movement;
- memory loss, loss of cognitive abilities;
- depression, distraction, irritability;
- slurred speech.
In some cases, the prognosis is disappointing, leading to disability, and sometimes death.
TIA Prevention
To prevent the occurrence of the disease, it is necessary:
- Increase physical activity. Moderate physical activity normalizes blood circulation, strengthens the immune system and stabilizes the respiratory system, reduces the risk of TIA. Preference is given to walking, swimming, therapeutic exercises, cycling and yoga.
- Follow a diet. Fatty, salty, smoked, spicy, canned foods should be limited in the diet. Give preference to cereals, vegetables and fruits. With high coagulability and a high concentration of sugar in the blood, seek the help of a dietitian to draw up a special nutrition program.
- Timely treatment of chronic diseases. With an exacerbation of any disease, timely support of the body with medicines prescribed by a doctor is required.
- Monitor blood pressure. If necessary, correct with medication.
- Refuse bad habits: smoking and alcohol.
- Elimination of risk factors. Systematically monitor cholesterol and blood coagulation. If necessary, urgently correct them.

Do not ignore the abnormal condition that occurred with TIA, over time it will worsen. This disease warns a person of an increased risk of stroke. Having listened to such a signal, the patient must prevent a subsequent deterioration in health and return to normal life.