Serous meningitis is a serious infectious pathology of the meninges. A misconception about the causes of this disease is common. Many people believe that meningitis appears due to being in the cold without a hat. However, this disease has an exclusively infectious origin. Most often it is caused by viruses. Hypothermia of the head can only be a provoking factor in the development of the inflammatory process.
Causative agents of the disease
With serous meningitis, inflammation affects the soft membrane of the brain, which is located closest to the surface of the organ. There are a large number of nerves and blood vessels, so the symptoms of pathology are pronounced and difficult to tolerate.
This disease is caused by various microorganisms. The most common cause of inflammation is the Coxsackie virus. Also in the etiology of serous meningitis, an important role is played by the causative agents of the following diseases:
- flu
- infectious mononucleosis;
- herpetic infection;
- measles
- rubella
- adenovirus infection ("stomach flu");
- mumps (mumps).
In rare cases, bacteria cause damage to the meninges: Koch's bacillus or pale treponema. This happens in patients with tuberculosis or syphilis. Infection enters the brain with blood flow. The disease can also be a result of damage to the body by Candida yeast. But such a pathology is rarely observed, mainly in people with sharply reduced immunity, for example, in HIV-infected people. Serous-viral meningitis is easier and has a more favorable prognosis than serous-bacterial.
Primary and secondary forms of pathology are distinguished. In the first case, the disease occurs if the infection immediately enters the brain from the outside. Secondary meningitis occurs as a complication of other ailments.
Transmission routes
The defeat of the soft meninges always occurs very quickly, the symptoms of the disease are rapidly increasing. Most often, microorganisms called Koksaki become the cause of serous-viral meningitis. These viruses live in the intestines (hence the name enteroviruses), but do not lead to gastrointestinal damage, but to general intoxication of the body. They can cause an infectious disease with fever and a rash (hand-foot-mouth syndrome), but damage to the central nervous system often occurs.
Viral infection, which leads to inflammation of the meninges, spreads in the following ways:
- Airborne. If viruses accumulate on the mucous membrane of the respiratory tract, then a person releases them during coughing, sneezing and talking.
- Contact way. Microorganisms are on the skin and move to various objects. Using common things with a sick person, you can easily become infected. The disease often spreads through dirty fruits and vegetables, as well as through unwashed hands.
- Through the water. Outbreaks of enterovirus infections are common in resorts where people bathe in shared pools. This microorganism may persist in the aquatic environment.
Most often, enterovirus infection occurs in the summer. Children are especially susceptible to infection. Adults are less likely to get sick.
There is also a special form of viral serous pathology - lymphocytic choriomeningitis. With it, inflammation affects not only the soft membranes, but also the vessels of the ventricles of the brain. This infection is spread by rodents - mice and rats. A person becomes infected by eating food and water contaminated with secretions of sick animals.
Provocative factors
If an infection enters the body, it does not always lead to serous-viral meningitis. For the onset of the disease, additional unfavorable conditions are necessary. The following factors can provoke the development of inflammation in the shells of the brain:
- Low immunity. This is the main cause of virus activity. Most often, people with a weakened body are prone to meningitis. These are patients with chronic diseases, various immunodeficiency states, as well as undergoing treatment with cytostatics and corticosteroids.
- Frequent viral infections. If the child is constantly cold, there is a high risk of getting a complication of the disease in the form of inflammation of the meninges.
- Hypothermia of the body. This factor does not play a major role in the occurrence of serous meningitis. Excessive exposure to cold can only indirectly affect the development of the disease. Usually hypothermia contributes to frequent colds, and meningitis occurs as a complication.
In childhood, the following circumstances can contribute to the development of meningitis:
- prematurity of the baby;
- intrauterine infection with rubella and other viral diseases;
- birth injuries;
- congenital insufficiency of immunity.
Such children have an increased risk of the disease.
The difference between the serous form of the disease and purulent
It is important to conduct a differential diagnosis of serous and purulent meningitis. This is necessary to choose the right treatment tactics. Two types of disease differ in etiology, pathological changes and clinical presentation. The serous form of meningitis is most often caused by viruses, with inflammation in the membranes of the brain formed not pus, but exudate (serous fluid). Nerve cells do not die.
The purulent form is most often associated with brain damage by meningococci. It is characterized by the death of neurons. Purulent contents appear in the membranes. This type of meningitis is much more difficult and has more dangerous consequences than serous. Diagnostic tests help distinguish one form of the disease from another.
Incubation period
The incubation period of serous meningitis can be different in duration. Its duration depends on the type of pathogen. For most viral infections, the latent period is 2 to 5 days. With rubella, it can increase up to 2 weeks. In children 2-6 years old, the incubation period can last 1-2 weeks.
At this time, a person does not feel any deviations in well-being. Only in young children under 1 year of age, some changes in behavior can be noticed. Kids often cry, are capricious, their appetite decreases and sleep is disturbed.
Common symptoms of the disease
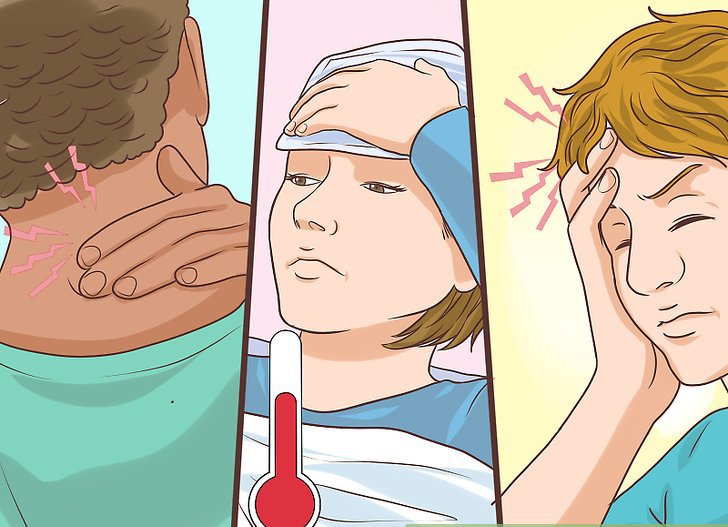
After the incubation period, an intermediate (prodromal) stage of the disease occurs. It is characterized by a slight fever, weakness, fatigue, and decreased appetite. After this, acute signs of serous meningitis develop:
- A severe headache occurs, which is localized in the temporal-frontal region and gives to the neck. Patients describe this sensation as extremely painful. With noise and bright light, pain intensifies. Analgesics do not help much.
- The temperature rises sharply (up to 40 degrees). The fever lasts 2-4 days, then decreases slightly. But after some time, the temperature rises again.
- Pain in the head is accompanied by nausea, severe vomiting "fountain" due to increased intracranial pressure and irritation of the vomiting center.
- A sick person does not tolerate bright lights and harsh sounds. His skin becomes very sensitive to touch. The condition improves somewhat when in a quiet, darkened room.
- The patient lies in a characteristic position: his legs are pulled up to his body, his hands are pressed to his chest, and his head is thrown back. In this position, it becomes somewhat easier for him.
- Signs of general intoxication appear: severe weakness and malaise, aching joints.
- There may be a slight blur of consciousness.
- If there are nerve damage, then there are violations of swallowing, movements and double vision.
Features of symptoms in children
In childhood, the signs of serous inflammation of the meninges have their own characteristics. In addition to the symptoms listed above, a child may have colds: cough, runny nose, sore throat. High fever is accompanied by seizures of limbs, delirium and hallucinations.
In infants, bulging and tension in the fontanel are noted. The child becomes irritable, whining, moody. The kid constantly screams in a monotonous voice, doctors call this sign "brain scream."
A rash with this disease usually does not appear, except in cases where meningitis occurs against a background of a viral infection with skin manifestations (measles, rubella).
Meningeal symptoms
The general manifestations of serous meningitis associated with intoxication of the body have been described above. But there are specific signs of this disease, which play an important role in the diagnosis. These include:
- Tension of the cervical and occipital muscles. The patient can not press his head to his chest due to increased muscle tone.
- Symptom Kernig. If in a lying position bend the patient’s leg, then there is a strong muscle tension. Sometimes the patient cannot even straighten the limb.
- Symptoms of Brudzinsky. When tilting the head, a person involuntarily pulls his legs to the body. This is a sign of irritation of the meninges. Also, when one leg is bent, the other limb is pulled to the body. These symptoms are not always observed with a serous form of the disease.
- Symptom Lesage. It is observed in children in infancy. If the child is lifted and held upright, then he bends his legs and pulls them to the body.
The doctor conducts the identification of these symptoms during a diagnostic examination of the patient.
Adult Complications
Severe consequences of serous meningitis in adults are rare. The disease can be complicated by pneumonia, inflammation of the heart membrane, arthritis. Sometimes vision or hearing is impaired. Perhaps the appearance of periodic pain and noise in the head.
The most dangerous complication of serous meningitis is the attachment of a bacterial infection and the transition of the disease into a purulent form. Also, inflammation can spread from the membranes of the brain to gray matter. To avoid such serious consequences, it is necessary to start treatment of the disease in a timely manner.
Complications in children
In childhood, complications occur more often than in adults. Pathology can adversely affect the development of the child. The following effects of serous meningitis in children are possible:
- mental retardation;
- hearing impairment;
- strabismus;
- blurred vision;
- trembling and involuntary movements of the eyeballs;
- epileptic seizures.
At the first signs of the disease, you must urgently call a doctor. Timely treatment will minimize the risk of complications.
Diagnostics
During the examination, the doctor determines the signs of damage to the meninges. The specialist identifies the symptoms of Kernig, Brudzinsky and Lesage (in children), as well as neck muscle tension.
An important role in the differential diagnosis of serous meningitis is played by spinal puncture. Under anesthesia, a long needle is punctured in the lumbar region. Spinal fluid (cerebrospinal fluid) is taken for analysis. Her research allows us to distinguish the serous form of the disease from purulent. If the cerebrospinal fluid protein is slightly increased and lymphocytes predominate, then this indicates viral meningitis. If the norms of protein content are greatly exceeded and the number of neutrophils is increased, then this indicates a purulent form of the disease.
Additionally, MRI and CT of the brain can be prescribed, as well as a blood test for viral infections.
Treatment methods
With serous inflammation of the meninges, the patient is urgently hospitalized. It is advisable to place the patient in a darkened room where there are no external stimuli (noise, bright light). Strict bed rest is recommended. In the hospital, drug treatment is carried out:
- To reduce the intoxication of the body, patients are given droppers with saline solutions, as well as with ascorbic acid and corticosteroids.
- To reduce intracranial pressure, diuretics are prescribed: Veroshpiron, Furosemide, Lasix.
- At high temperature, drugs with paracetamol and ibuprofen are prescribed.
- Antiviral therapy is carried out with interferon-type drugs. If meningitis is caused by the causative agent of herpes or infectious mononucleosis, then the use of "Acyclovir" is indicated.
- Antibiotics will not cure viral meningitis. But broad-spectrum antibacterial drugs are still used to prevent the development of a purulent form of the disease.
- For pain, the use of "No-Shp" is useful.
- If the child has cramps, then use the drugs "Domosedan" or "Seduxen".
- To strengthen the immune system, B vitamins and ascorbic acid are prescribed.
- If the disease is caused by a Koch bacillus, pale treponema or yeast, then the use of anti-tuberculosis, anti-syphilitic and antifungal agents is indicated.

In some cases, spinal punctures are used for therapeutic purposes. Removing part of the cerebrospinal fluid helps to reduce intracranial pressure and reduce headache.
At the stage of recovery, patients are prescribed nootropic drugs (Piracetam, Nootropil, Glycine), as well as drugs with succinic acid. This helps to restore the brain after an illness.
Disease prognosis
The prognosis for serous meningitis of a viral etiology is usually favorable. Improving the patient's condition with proper treatment occurs in 5-6 days. The disease lasts about 2 weeks, after which comes a complete recovery.
If serous inflammation is caused by tuberculosis bacteria or yeast, then it requires a long and persistent treatment. Such forms of the disease often recur.
With complications and the transition of the disease into a purulent form, as well as with the spread of pathology to the substance of the brain, the prognosis significantly worsens.
Prevention
Currently, specific prevention of this disease has not been developed. To protect yourself from serous inflammation of the meninges, it is necessary to protect your body from infections. Contact with patients with viral pathologies should be avoided, as well as strengthening immunity. If an outbreak of enteroviral diseases is observed in the summer, swimming in closed ponds should be avoided.
It is impossible to vaccinate against the serous form of the disease, since it is caused by viruses of various kinds. The Mentsevax vaccine is ineffective in this case. It is designed to protect against purulent meningitis, which is caused by meningococci. You can only take a course of vaccinations against various viral infections (measles, rubella, flu). This will slightly reduce the risk of the disease. However, enteroviruses often become the causative agent of inflammation, and there are no vaccines against them yet.