Focal segmental glomerulosclerosis (FSH) is the leading cause of kidney disease worldwide. The presumed etiology of primary FSHC is a plasma factor with reactivity to immunosuppressive therapy and a risk of relapse after kidney transplantation. Adaptive FSGS is associated with excessive nephron loading due to increased body size, decreased nephron capacity, or single glomerular hyperfiltration associated with certain diseases.
Introduction
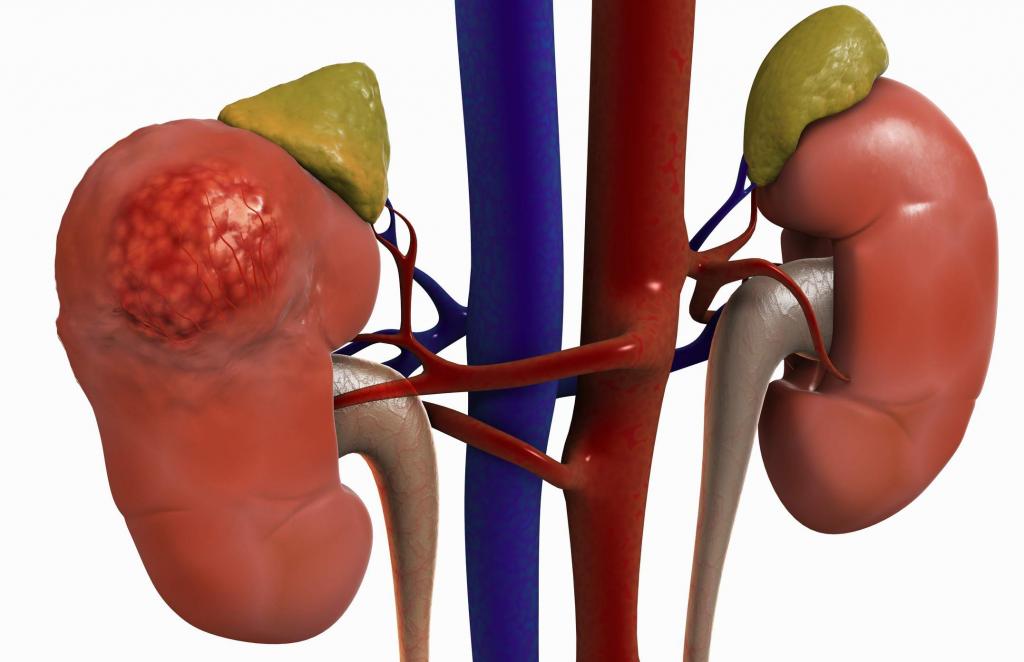
Focal segmental glomerulosclerosis is a leading glomerular cause of renal failure. He refers to a histological picture that characterizes 6 possible underlying etiologies, sharing the general theme of bruising and depletion of podocytes.
Diagnosis of focal segmental glomerulosclerosis relies on the integration of clinical history (family diseases, birth history, peak weight and body weight, benefit of the drug), laboratory clinical findings (serum albumin, urine protein, and viral serologies) and renal histopathology. Proteinuria may be in the nephrotic or subnephrotic range. Of decisive importance is the elimination of other systemic diseases or primary pathologies of the kidneys, which may lead to a similar presentation.
Epidemiology and the global burden
The prevalence of focal segmental glomerulosclerosis, compared with other diagnoses of such diseases, is growing worldwide. However, the absolute frequency and prevalence is difficult to establish, given the large global differences in the indications, availability, and pathological support of kidney biopsy.
A review of published literature around the world was carried out, which shows that the annual incidence rate ranges from 0.2 to 1.8 per 100,000 population per year. The average incidence rate was 2.7 patients per million. There is a significant racial and ethnic predisposition. In addition, the symptoms of renal failure in women are less pronounced than in men.
Typology
The classification of focal segmental glomerulosclerosis is multifaceted. It includes pathophysiological, histological and genetic aspects. Initially, FSGS was divided into primary (idiopathic) and secondary forms. The latter can include family (genetic), virus-associated, drug-induced forms.
Clinical recommendations for focal segmental glomerulosclerosis may relate to the histological variant, primarily to the glucocorticoid reactivity of the tip lesion and the aggressive, implacable nature of the collapsing variants.
6 clinical forms
Combining genetic susceptibility, pathophysiological factors, clinical history and response to therapy, it is advisable to group FSGS into six clinical forms. They include:
- primary;
- adaptive;
- highly genetic;
- virus-mediated;
- drug related;
- APOL1-linked.
Histopathology of the disease
Minimal symptoms of glomerulonephritis in adults are manifested by the absence of tubulointerzital scarring. The defeat of the tip is the focal adhesion of the glomerular bundle to the Bowman capsule near the proximal take-off of the tubule.
The most characteristic option is collapsing. A specific example can be evaluated in the installation of endothelial tubule reticular inclusions observed in ultrastructural analysis. They can be observed in high states of interferons, including viral infection. Minimum disease change and tip damage are the most responsive and least progressive, and collapsing glomerulopathies, resistant to therapy and rapidly progressing.
Symptoms indicating ailment
Signs and symptoms of glomerulonephritis in adults depend on the presence of an acute or chronic form. They include:
- Pink or brown colored urine due to increased red blood cell count (hematuria).
- Foamy urine due to excess protein (proteinuria).
- High blood pressure (hypertension).
- Fluid retention (edema). It appears on the face, arms, legs and stomach.
Separately, the symptoms of renal failure in women are distinguished:
- Decreased urine output.
- Fluid retention causing swelling of the legs.
- Dyspnea.
- Fatigue.
- Confused consciousness.
- Nausea.
- Weakness.
- Irregular heartbeat.
- Pain in the kidney area.
- Fainting or coma in severe cases.
The surest way to identify FSGS
The first thing to do is a kidney urine test. It includes two tests:
- The ratio of albumin to creatinine. Too much albumin in urine is an early sign of kidney damage. Three positive results for three months or more is a sign of illness.
- Glomerular filtration rate. Blood is tested for waste called creatinine. It comes from muscle tissue. When the kidneys are damaged, problems arise with the removal of creatinine from the blood. The test result is used in a mathematical formula with age, race and gender to find out the glomerular filtration rate.
Main reasons
Conditions that can lead to inflammation of the glomeruli of the kidney are:
- Infectious diseases. Glomerulonephritis can develop 7-14 days after previous skin infections (impetigo) or streptococcal throat infections. To fight them, the body is forced to produce many additional antibodies, which are able to eventually settle in the glomeruli, causing inflammation.
- Bacterial endocarditis. Bacteria can spread through the bloodstream and settle in the heart, causing infection of one or more heart valves. Bacterial endocarditis is associated with glomerular disease, but the relationship between them is unclear.
- Viral infection. Human Immunodeficiency Virus (HIV), Hepatitis B and C can cause disease.
- Lupus. It can affect many organs and parts of the body, including blood cells, skin, kidneys, heart, joints, and lungs.
- Goodpasture Syndrome. This is a rare lung disease that mimics pneumonia. It can cause glomerulonephritis and bleeding in the lungs.
- Nephropathy This primary glomerular disease occurs due to glomerular immunoglobulin deposits. It can progress for years without noticeable symptoms.
Additional reasons
Additional causes of the disease include:
- Polyarteritis. This form of vasculitis affects small and medium blood vessels. Known as Wegener's granulomatosis.
- High blood pressure. Kidney function is declining. They process sodium worse.
- Focal segmental glomerulosclerosis. It is characterized by diffuse scarring of some glomeruli. This condition may be the result of another disease or may occur for an unknown reason.
- Diabetic kidney disease (diabetic nephropathy).
- Alport Syndrome. Inherited form. It may also impair hearing or vision.
- Multiple myeloma, lung cancer, and chronic lymphocytic leukemia.
Disease mechanism
Focal segmental glomerulosclerosis is a diverse syndrome that occurs after trauma to podocytes for various reasons. Sources of damage are different:
- circulating factors;
- genetic abnormalities;
- viral infection;
- drug treatment.
For the most part, the interaction between these drivers is unclear and complex. For example, adaptive FSGS includes both podocyte stress (mismatch between glomerular load and glomerular capacity) and genetic susceptibility.
Damage to podocytes from any form of FSHC (or from other glomerular diseases) initiates the process leading to acute nephritic syndrome. A progressive loss of damaged podocytes into the urinary space occurs. To balance the deficit, these cells compensate for hypertrophy, covering the surface of the glomerular capillaries.
With adaptive FSGS, glomerular hypertrophy occurs at the beginning of the disease process. In other forms, glomerular hypertrophy occurs with progressive loss of the nephron. This leads to increased pressures and currents in the remaining glomeruli of the patent.
The following sections discuss pathological mechanisms, therapy, and treatment of focal segmental glomerulosclerosis.
Primary FSGS
Includes genetic, viral, and drug-related FSGS. The mechanism of damage to podocytes includes a circulating factor, possibly a cytokine, which makes specific patients susceptible. This is the most common form in adolescents and young adults. It is commonly associated with nephrotic series proteinuria (sometimes massive), decreased plasma albumin levels, and hyperlipidemia.
Currently, primary FSHC therapy is based on immunosuppressive agents. These are glucocorticoids and calcineurin inhibitors that directly modulate the phenotype of podocytes. Recurrent FSHS remain a clinical problem. Only one of the 77 initial kidney biopsies in patients who subsequently relapsed showed a perigular variant. Plasma exchange therapy may cause temporary remission.
Adaptive FSGS
It occurs after a period of glomerular hyperfiltration at the level of the nephron and hypertension after pathophysiology. Conditions that are associated with its development include:
- congenital cyanotic heart disease;
- sickle cell anemia;
- obesity;
- androgen abuse;
- sleep apnea;
- high protein diet.
The duration of single-glomerular hyperfiltration is usually measured decades before glomerulosclerosis progresses. Adaptive FSGS leads to progressive glomerular hypertrophy cycles, stress and exhaustion, excessive deposition of the extracellular matrix in the glomerulus. Diagnostic features of a kidney biopsy include large glomeruli, a predominance of perigular scars showing sclerotic changes. Clinical features include regular serum albumin, which is unusual in primary FSHS.
Genetic FSGS
It takes two forms. Some patients with a certain genetic predisposition will develop the disease, while others will not. The number of genes associated with FSHC is growing every year, largely due to the spread of sequencing of the entire exome. To date, at least 38 have been identified.
Some genes are associated with a syndrome that includes extrarenal manifestations. This may provide a clinical clue that a patient may have a mutation in a particular gene. Others are associated with characteristic changes in the morphology of the basement membrane or the morphology of mitochondria.
If the family has not previously undergone genetic testing, the most effective approach is to use panels that focus on early FSGS (infants and children). Genetic test resources around the world are available at the National Center for Biotechnology Information and National Institutes of Health.